|
Vocapedia >
Health >
Mental health >
Psychiatry
Psychiatrists, DSM

Dr. Darrel A. Regier
is co-chairman of a panel compiling the latest
Diagnostic and Statistical Manual of Mental Disorders
Photograph: Brendan Smialowski
for The New York Times
Psychiatrists Revising the Book
of Human Troubles
NYT
18 December 2008
https://www.nytimes.com/2008/12/18/
health/18psych.html
psychiatry UK
https://www.theguardian.com/society/
psychiatry
psychiatry
USA
https://www.propublica.org/article/
mental-health-suicide-highmark-bcbs-insurance-denials - September 10, 2025
https://www.nytimes.com/2025/03/17/
health/laura-delano-psychiatric-meds.html
https://www.nytimes.com/2024/10/20/
health/los-angeles-homeless-psychiatry.html
https://www.nytimes.com/2024/05/21/
health/psychiatric-restraint-forced-medication.html
https://www.nytimes.com/2021/05/09/
health/psychedelics-mdma-psilocybin-molly-mental-health.html
https://www.npr.org/sections/health-shots/2024/01/27/
1227062470/keto-ketogenic-diet-mental-illness-bipolar-depression
https://www.npr.org/2019/11/18/
780563160/how-1-study-changed-the-field-of-psychiatry-forever
https://www.npr.org/sections/health-shots/2019/09/09/
746950433/telepsychiatry-helps-recruitment-and-patient-care-in-rural-areas
https://www.npr.org/2019/04/24/
716744558/how-psychiatry-turned-to-drugs-to-treat-mental-illness
http://www.nytimes.com/2016/08/09/
health/psychiatrist-holistic-mental-health.html
http://www.nytimes.com/2015/07/19/
opinion/psychiatrys-identity-crisis.html
http://www.npr.org/sections/health-shots/2013/05/16/
184454931/why-is-psychiatrys-new-manual-so-much-like-the-old-one
http://opinionator.blogs.nytimes.com/2013/02/06/
the-limits-of-psychiatry/
http://www.nytimes.com/2011/04/21/
health/21freedman.html
http://www.nytimes.com/2011/03/09/
opinion/l09psych.html
http://www.nytimes.com/2011/03/06/
health/policy/06doctors.html
forensic psychiatry UK
https://www.theguardian.com/society/2021/jun/17/
inside-the-mind-of-murderer-
power-and-limits-of-forensic-psychiatry-crime-prison
telepsychiatry
USA
https://www.npr.org/sections/health-shots/2019/09/09/
746950433/telepsychiatry-helps-recruitment-and-patient-care-
in-rural-areas
https://www.npr.org/sections/health-shots/2014/05/07/
308749287/telepsychiatry-brings-emergency-mental-health-care-
to-rural-areas/
American Psychiatric Association
USA
https://www.nytimes.com/2024/05/21/
health/psychiatric-restraint-forced-medication.html
psychiatric hospitals
USA
https://www.propublica.org/article/
psychiatric-hospitals-emtala-mental-health-profit - September 23, 2025
antipsychiatry
UK / USA
https://www.nytimes.com/2012/09/12/
health/dr-thomas-szasz-psychiatrist-who-led-movement-against-his-field-
dies-at-92.html
https://www.theguardian.com/books/2012/sep/02/
rd-laing-mental-health-sanity
https://www.theguardian.com/society/2012/oct/04/
thomas-szasz
psychiatrist UK
https://www.theguardian.com/society/2013/may/12/
psychiatrists-under-fire-mental-health
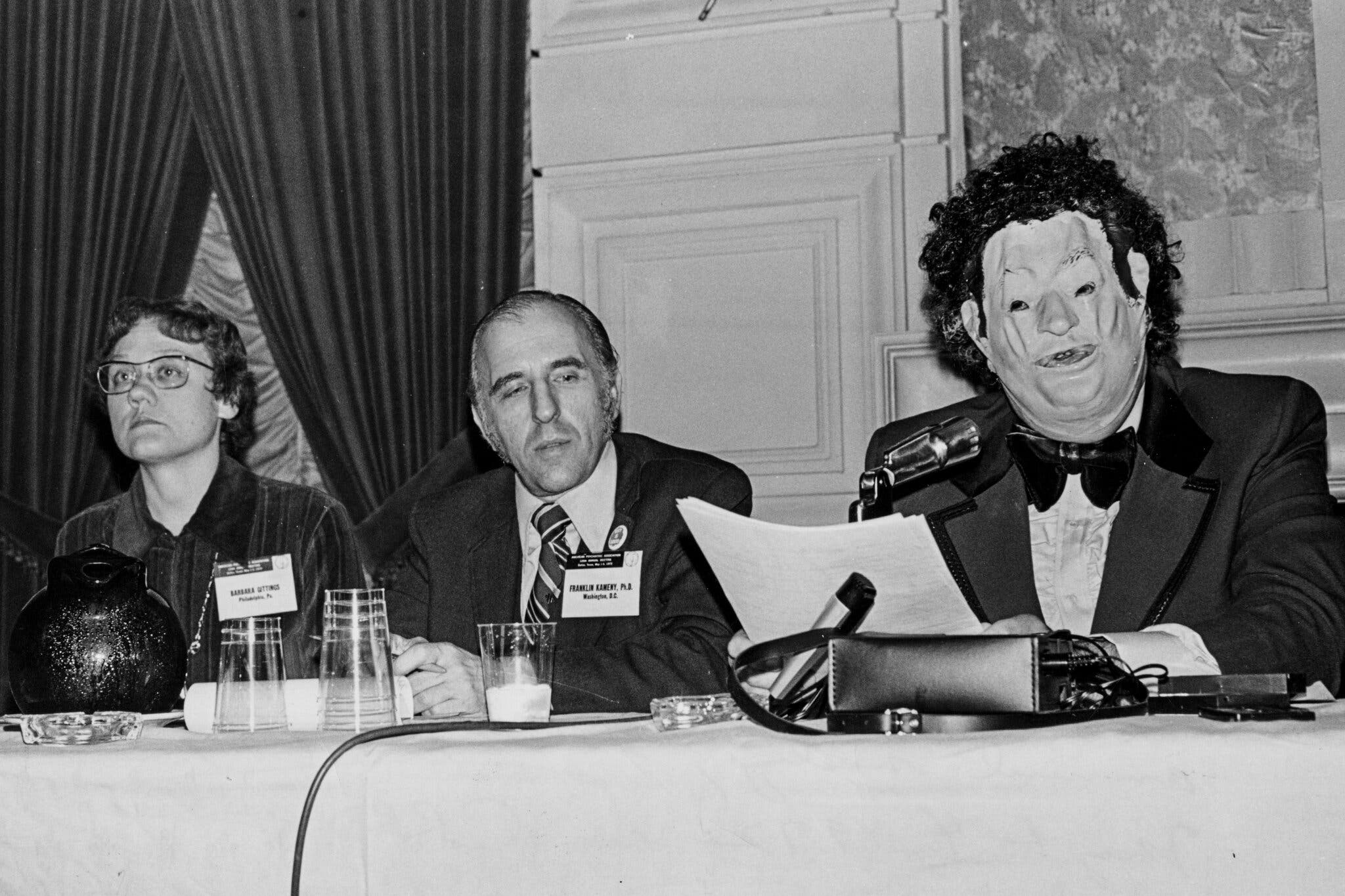
Dr. John Fryer,
a.k.a. “Dr. Henry Anonymous,” right,
during the 1972 convention
of the American Psychiatric
Association in Dallas.
Photograph: Kay Tobin,
via Manuscripts and Archives Division,
The New York Public
Library
He Spurred a Revolution in Psychiatry.
Then He ‘Disappeared.’
In 1972,
Dr. John Fryer risked his career to tell his colleagues
that gay people were not mentally ill.
His act sent ripples through the legal, medical
and justice
systems.
NYT
Published May 2, 2022
Updated May 6, 2022
https://www.nytimes.com/2022/05/02/
health/john-fryer-psychiatry.html
USA > psychiatrist
UK / USA
https://www.propublica.org/article/
mental-health-suicide-highmark-bcbs-insurance-denials - September 10, 2025
https://www.nytimes.com/2023/12/18/
us/jeanne-hoff-dead.html
https://www.nytimes.com/2022/05/02/
health/john-fryer-psychiatry.html
https://www.npr.org/sections/health-shots/2019/09/09/
746950433/telepsychiatry-helps-recruitment-and-patient-care-in-rural-areas
https://www.nytimes.com/2019/07/11/
well/live/chasing-my-shadow-as-a-cancer-patient-in-talk-therapy.html
https://www.nytimes.com/2017/11/30/
opinion/psychiatrists-trump.html
https://www.nytimes.com/2017/10/11/
opinion/psychiatrists-mass-killers.html
http://www.npr.org/sections/thetwo-way/2017/07/25/
539238529/goldwater-rule-still-in-place-
barring-many-psychiatrists-from-commenting-on-trum
http://www.nytimes.com/2015/05/26/
health/rural-nebraska-offers-stark-view-of-nursing-autonomy-debate.html
http://www.nytimes.com/2013/10/06/
opinion/sunday/great-betrayals.html
http://www.npr.org/sections/health-shots/2013/05/16/
184454931/why-is-psychiatrys-new-manual-so-much-like-the-old-one
https://www.theguardian.com/society/2012/oct/04/
thomas-szasz
http://www.nytimes.com/2010/05/05/us/
05greenspan.html
http://www.nytimes.com/2010/04/19/us/
19masterson.html
http://www.nytimes.com/2009/06/23/
health/23mind.html
Dr. Robert L. Spitzer
USA
considered by some
to be the father of modern psychiatry
http://www.nytimes.com/2012/05/19/
health/dr-robert-l-spitzer-noted-psychiatrist-apologizes-for-study-on-gay-cure.html
Charles Silverstein USA
1935-2023
psychologist and therapist
who played a key role in getting homosexuality
declassified as a mental illness,
https://www.npr.org/2023/02/09/
1155847480/charles-silverstein-psychologist-
declassify-homosexuality-mental-illness
Yehuda Nir USA 1930-2014
psychiatrist
whose childhood was
shaped
by having to masquerade
as a Roman
Catholic
in German-occupied Poland
to
escape Nazi persecution,
an ordeal that he turned
into a
well-received memoir
and that guided him
in treating
victims of trauma
http://www.nytimes.com/2014/07/20/
health/yehuda-nir-a-psychiatrist-and-holocaust-survivor-dies-at-84.html
psychiatrist USA
https://www.npr.org/2024/04/02/
1242170517/our-kids-are-not-ok-child-psychiatrist-harold-koplewicz-says
Thomas Szasz USA 1920-2012
psychiatrist
whose 1961 book
“The Myth of Mental Illness”
questioned the legitimacy of his field
and provided the intellectual grounding
for generations of critics,
patient advocates
and antipsychiatry activists,
making enemies of many fellow doctors
https://www.nytimes.com/2012/09/12/
health/dr-thomas-szasz-psychiatrist-who-led-movement-against-his-field-
dies-at-92.html
https://www.nytimes.com/2012/09/12/
health/dr-thomas-szasz-psychiatrist-who-led-movement-against-his-field-
dies-at-92.html
https://www.theguardian.com/society/2012/oct/04/
thomas-szasz
James Griffith Edwards USA 1928-2012
psychiatrist who helped establish
addiction medicine as a science,
formulating definitions
of drug and alcohol dependence
that are used worldwide
to diagnose and treat substance abuse
http://www.nytimes.com/2012/09/26/
health/dr-griffith-edwards-pioneer-in-addiction-medicine-dies-at-83.html
Thomas Szasz USA 1920-2012
psychiatrist
whose 1961 book
“The Myth of Mental Illness”
questioned the legitimacy of his field
and provided the intellectual grounding
for generations of critics,
patient advocates
and antipsychiatry activists,
making enemies of many fellow doctors
https://www.nytimes.com/2012/09/12/
health/dr-thomas-szasz-psychiatrist-who-led-movement-against-his-field-
dies-at-92.html
https://www.nytimes.com/2012/09/12/
health/dr-thomas-szasz-psychiatrist-who-led-movement-against-his-field-
dies-at-92.html
https://www.theguardian.com/society/2012/oct/04/
thomas-szasz
John Ercel Fryer USA
1937-2003
In 1972,
Dr. John Fryer risked his career
to tell his colleagues
that gay people were not mentally ill.
His act sent ripples
through the legal, medical and justice systems.
https://www.nytimes.com/2022/05/02/
health/john-fryer-psychiatry.html
mental disorders / mental health
disorders
USA
http://www.nytimes.com/2014/11/24/us/
debate-persists-over-diagnosing-mental-health-disorders-long-after-sybil.html
http://www.nytimes.com/2013/03/01/health/
study-finds-genetic-risk-factors-shared-by-5-psychiatric-disorders.html
borderline personality disorder
USA
personality disorder
USA
http://www.nytimes.com/2010/04/19/us/19masterson.html
mental disorders on campus
USA
http://www.nytimes.com/roomfordebate/2011/01/12/
dealing-with-mental-disorders-on-campus
eating disorders
USA
http://www.nytimes.com/2011/10/14/
business/ruling-offers-hope-to-eating-disorder-sufferers.html
eating disorders > Anorexia
Nervosa
eating disorders > Bulimia
narcissism
USA
http://www.nytimes.com/2010/04/19/us/
19masterson.html
narcissistic personality disorder
lack
empathy UK
https://www.theguardian.com/commentisfree/2016/nov/12/
donald-trump-king-narcissist-victory
lack of empathy
USA
https://www.nytimes.com/2017/02/14/
opinion/an-eminent-psychiatrist-demurs-on-trumps-mental-state.html
psychosis
UK
http://www.independent.co.uk/life-style/health-and-families/
features/living-with-psychosis-im-mad-but-not-bad-2025012.html
hypochondria
USA
http://www.nytimes.com/2013/01/13/
opinion/sunday/hypochondria-an-inside-look.html
psychiatric
medication
USA
https://www.nytimes.com/2025/03/17/
health/laura-delano-psychiatric-meds.html
medication
USA
https://www.nytimes.com/2013/09/30/
opinion/psychotherapys-image-problem.html
https://www.nytimes.com/2013/05/26/
opinion/sunday/sunday-dialogue-treating-mental-illness.html
meds USA
https://www.nytimes.com/2020/04/28/
opinion/coronavirus-anxiety-medication.html
FRONTLINE > The Medicated Child
Aired: 01/08/2008 56:10 Rating: NR
Millions of U.S. children are taking psychiatric drugs,
most never tested on
kids.
Good medicine - or an uncontrolled experiment?
https://www.pbs.org/video/frontline-the-medicated-child/
psychiatric disorders
USA > Diagnostic
and Statistical
Manual of Mental Disorders DSM
UK / USA
https://www.psychiatry.org/
psychiatrists/practice/dsm
https://www.theguardian.com/society/2023/feb/25/
this-feels-more-like-spin-the-bottle-than-science-
my-mission-to-find-a-proper-diagnosis-and-treatment-for-my-sons-psychosis
https://www.nytimes.com/2017/02/14/
opinion/an-eminent-psychiatrist-demurs-on-trumps-mental-state.html
https://www.theguardian.com/commentisfree/2016/nov/30/
diagnosed-donald-trump-goldwater-rule-mental-health
http://www.theguardian.com/science/2013/aug/04/truly-madly-deeply-delusional
http://www.npr.org/2013/05/31/
187534467/bad-diagnosis-for-new-psychiatry-bible
http://www.nytimes.com/2013/05/28/
opinion/brooks-heroes-of-uncertainty.html
https://www.theguardian.com/science/political-science/2013/may/28/
politics-psychiatry
http://www.npr.org/sections/health-shots/2013/05/16/
184454931/why-is-psychiatrys-new-manual-so-much-like-the-old-one
http://www.guardian.co.uk/society/2013/may/12/psychiatrists-under-fire-mental-health
https://www.nytimes.com/2013/05/07/
health/psychiatrys-new-guide-falls-short-experts-say.html
http://www.nytimes.com/2012/05/12/
opinion/break-up-the-psychiatric-monopoly.html
http://www.nytimes.com/2012/05/09/
health/dsm-panel-backs-down-on-diagnoses.html
http://www.npr.org/2012/12/04/1
66503627/the-challenges-posed-by-personality-disorders
http://www.nytimes.com/2008/12/18/health/18psych.html
http://www.npr.org/templates/story/
story.php?storyId=1400925 - 18 August 2003
psychiatric name-calling USA
https://www.nytimes.com/2017/02/14/
opinion/an-eminent-psychiatrist-demurs-on-trumps-mental-state.html
recovery
USA
https://www.nytimes.com/2020/02/25/
health/mental-health-depression-recovery.html
Corpus of news articles
Health > Mental health > Therapists
Psychologists, Psychoanalysts,
Psychiatrists, DSM, Therapy
Maurice
M. Rapport,
Who Studied Serotonin,
Dies at 91
September
2, 2011
The New York Times
By WILLIAM GRIMES
Maurice M.
Rapport, a biochemist who helped isolate and name the neurotransmitter
serotonin, which plays a role in regulating mood and mental states, and who
first described its molecular structure, a development that led to the creation
of a wide variety of psychiatric and other drugs, died on Aug. 18 in Durham,
N.C. He was 91.
The death was confirmed by his daughter, Erica Rapport Gringle.
In the 1940s Dr. Rapport (pronounced RA-port) was a freshly minted biochemist
from the California Institute of Technology when he began working at the
Cleveland Clinic Foundation with Irvine H. Page, a leading specialist on high
blood pressure and cardiovascular disease.
Scientists had known since the 1860s of a substance in the serum released during
clotting that constricts blood vessels by acting on the smooth muscles of the
blood-vessel walls. In the 20th century, researchers pinpointed its source in
blood platelets, but its identity remained a mystery.
Dr. Rapport, working with Dr. Page and Arda A. Green, isolated the substance
and, in a paper published in 1948, gave it a name: serotonin, derived from
“serum” and “tonic.”
On his own, Dr. Rapport identified the structure of serotonin as
5-hydroxytryptamine, or 5-HT, as it is called by pharmacologists. His findings,
published in 1949, made it possible for commercial laboratories to synthesize
serotonin and study its properties as a neurotransmitter.
More than 90,000 scientific papers have been published on 5-HT, and the
Serotonin Club, a professional organization, regularly holds conferences to
report on research in the field.
Initially, researchers focused on agents to block serotonin, which, by
constricting blood vessels, causes blood pressure to rise. After researchers
discovered its presence in the brain, and its chemical similarity to LSD, which
mimics serotonin in the brain, they began focusing on serotonin’s role in
regulating mood and mental functioning.
Further research showed that serotonin also plays a critical role in the central
nervous system — where it helps regulate mood, appetite, sex and sleep — and the
gut.
This new understanding of the structure and functioning of serotonin led to a
changing view of mental disorders as chemical imbalances and opened the way to
the development of antidepressants and antipsychotic drugs that act on 5-HT, as
well as drugs for treating cardiovascular and gastrointestinal disease.
Maurice Rapoport was born on Sept. 23, 1919, in Atlantic City. His father, a
furrier who had emigrated from Russia, left the family when Maurice was a small
child. His mother changed the spelling of the family name and Maurice later
adopted the middle initial “M,” although it did not stand for anything.
After graduating from DeWitt Clinton High School in the Bronx, he earned a
bachelor’s degree in chemistry from City College in 1940 and a doctorate in
organic chemistry from Cal Tech in 1946. For his work on serotonin he was
awarded a Fulbright Scholarship in 1952 to study with Dr. Daniel Bovet, later a
Nobel Prize winner for his work in pharmacology, at the Istituto Superiore di
Sanità in Rome.
After doing research in biochemistry at Columbia, immunology at the
Sloan-Kettering Institute for Cancer Research and biochemistry at the Albert
Einstein College of Medicine, Dr. Rapport joined the staff of the New York
Psychiatric Institute, where he created the division of neuroscience by
combining the old divisions of chemistry, pharmacology and bacteriology. He also
held the post of professor of biochemistry at Columbia’s College of Physicians
and Surgeons.
Dr. Rapport retired in 1986 and was a visiting professor in the neurology
department of the Albert Einstein College of Medicine until his death.
Dr. Rapport did important research on cancer, cardiovascular disease,
connective-tissue disease and demyelinating diseases, a type of nervous-system
disorder that includes multiple sclerosis.
One productive area of his research focused on the immunological activity of
lipids found in the nervous system, notably cytolipin H, which he isolated from
human cancer tissue in 1958. He also identified the lipid galactocerebroside as
the substance responsible for producing antigens specific to the brain, a
finding that led to a better understanding of the immune system.
Dr. Rapport’s wife, Edith, died in 1988. He lived in Hastings-on-Hudson with his
longtime companion, Nancy Reich, who survives him, before failing health made it
necessary for him to move in with his daughter, Erica, in Durham, in July. Other
survivors are his son, Ezra, of Oakland, Calif.; five grandchildren; and a
great-granddaughter.
Maurice M. Rapport, Who Studied Serotonin, Dies at 91,
NYT, 2.9.2011,
http://www.nytimes.com/2011/09/03/health/03rapport.html
Alfred
Freedman,
a Leader in Psychiatry,
Dies at 94
April 20,
2011
The New York Times
By WILLIAM GRIMES
Dr. Alfred
M. Freedman, a psychiatrist and social reformer who led the American Psychiatric
Association in 1973 when, overturning a century-old policy, it declared that
homosexuality was not a mental illness, died on Sunday in Manhattan. He was 94.
The cause was complications of surgery to treat a fractured hip, his son Dan
said.
In 1972, with pressure mounting from gay rights groups and from an increasing
number of psychiatrists to destigmatize homosexuality, Dr. Freedman was elected
president of the association, which he later described as a conservative “old
boys’ club.” Its 20,000 members were deeply divided about its policy on
homosexuality, which its Diagnostic and Statistical Manual of Mental Disorders
II classified as a “sexual deviation” in the same class as fetishism, voyeurism,
pedophilia and exhibitionism.
Well known as the chairman of the department of psychiatry at New York Medical
College and a strong proponent of community-oriented psychiatric and social
services, Dr. Freedman was approached by a group of young reformers, the
Committee of Concerned Psychiatrists, who persuaded him to run as a petition
candidate for the presidency of the psychiatric association.
Dr. Freedman, much to his surprise, won what may have been the first contested
election in the organization’s history — by 3 votes out of more than 9,000 cast.
Immediately on taking office, he threw his support behind a resolution, drafted
by Robert L. Spitzer of Columbia University, to remove homosexuality from the
list of mental disorders.
On Dec. 15, 1973, the board of trustees, many of them newly elected younger
psychiatrists, voted 13 to 0, with two abstentions, in favor of the resolution,
which stated that “by itself, homosexuality does not meet the criteria for being
a psychiatric disorder.”
It went on: “We will no longer insist on a label of sickness for individuals who
insist that they are well and demonstrate no generalized impairment in social
effectiveness.”
The board stopped short of declaring homosexuality “a normal variant of human
sexuality,” as the association’s task force on nomenclature had recommended.
The recently formed National Gay Task Force (now the National Gay and Lesbian
Task Force) hailed the resolution as “the greatest gay victory,” one that
removed “the cornerstone of oppression for one-tenth of our population.” Among
other things, the resolution helped reassure gay men and women in need of
treatment for mental problems that doctors would not have any authorization to
try to change their sexual orientation, or to identify homosexuality as the root
cause of their difficulties.
An equally important companion resolution condemned discrimination against gays
in such areas as housing and employment. In addition, it called on local, state
and federal lawmakers to pass legislation guaranteeing gay citizens the same
protections as other Americans, and to repeal all criminal statutes penalizing
sex between consenting adults.
The resolution served as a model for professional and religious organizations
that took similar positions in the years to come.
“It was a huge victory for a movement that in 1973 was young, small, very
underfunded and had not yet had this kind of political validation,” said Sue
Hyde, who organizes the annual conference of the National Gay and Lesbian Task
Force. “It is the single most important event in the history of what would
become the lesbian, gay, bisexual and transgender movement.”
In a 2007 interview Dr. Freedman said, “I felt at the time that that decision
was the most important thing we accomplished.”
Alfred Mordecai Freedman was born on Jan. 7, 1917, in Albany. He won
scholarships to study at Cornell, where he earned a bachelor’s degree in 1937.
He earned a medical degree from the University of Minnesota in 1941 but cut
short his internship at Harlem Hospital to enlist in the Army Air Corps.
During World War II he served as a laboratory officer in Miami and chief of
laboratories at the Air Corps hospital in Gulfport, Miss. He left the corps with
the rank of major.
After doing research on neuropsychology with Harold E. Himwich at Edgewood
Arsenal in Maryland, he became interested in the development of human cognition.
He underwent training in general and child psychiatry and began a residency at
Bellevue Hospital in Manhattan, where he became a senior child psychiatrist.
He was the chief psychiatrist in the pediatrics department at the Downstate
College of Medicine of the State University of New York for five years before
becoming the first full-time chairman of the department of psychiatry at New
York Medical College, then in East Harlem and now in Valhalla, N.Y.
In his 30 years at the college he built the department into an important
teaching institution with a large residency program. He greatly expanded the
psychiatric services offered at nearby Metropolitan Hospital, which is
affiliated with the school and where he was director of psychiatry.
To address social problems in East Harlem, Dr. Freedman created a treatment
program for adult drug addicts at the hospital in 1959 and the next year
established a similar program for adolescents. These were among the earliest
drug addiction programs to be conducted by a medical school and to be based in a
general hospital. He also founded a division of social and community psychiatry
at the school to serve neighborhood residents.
With Harold I. Kaplan, he edited “Comprehensive Textbook of Psychiatry,” which
became adopted as a standard text on its publication in 1967 and is now in its
ninth edition.
During his one-year term as president of the American Psychiatric Association,
Dr. Freedman made the misuse of psychiatry in the Soviet Union one of the
organization’s main issues. He challenged the Soviet government to answer
charges that it routinely held political dissidents in psychiatric hospitals,
and he led a delegation of American psychiatrists to the Soviet Union to visit
mental hospitals and confer with Soviet psychiatrists.
After retiring from New York Medical College, Dr. Freedman turned his attention
to the role that psychiatry played in death penalty cases. With his colleague
Abraham L. Halpern, he lobbied the American Medical Association to enforce the
provision in its code of ethics barring physicians from taking part in
executions, and he campaigned against the practice of using psychopharmacologic
drugs on psychotic death-row prisoners so that they could be declared competent
to be executed.
In addition to his son Dan, of Silver Spring, Md., he is survived by his wife,
Marcia; another son, Paul, of Pelham, N.Y.; and three grandchildren.
Alfred Freedman, a Leader in Psychiatry, Dies at 94, NYT,
20.4.2011,
http://www.nytimes.com/2011/04/21/health/21freedman.html
Talk Doesn’t Pay,
So Psychiatry Turns
to Drug Therapy
March 5, 2011
The New York Times
By GARDINER HARRIS
DOYLESTOWN, Pa. — Alone with his psychiatrist, the patient confided that his
newborn had serious health problems, his distraught wife was screaming at him
and he had started drinking again. With his life and second marriage falling
apart, the man said he needed help.
But the psychiatrist, Dr. Donald Levin, stopped him and said: “Hold it. I’m not
your therapist. I could adjust your medications, but I don’t think that’s
appropriate.”
Like many of the nation’s 48,000 psychiatrists, Dr. Levin, in large part because
of changes in how much insurance will pay, no longer provides talk therapy, the
form of psychiatry popularized by Sigmund Freud that dominated the profession
for decades. Instead, he prescribes medication, usually after a brief
consultation with each patient. So Dr. Levin sent the man away with a referral
to a less costly therapist and a personal crisis unexplored and unresolved.
Medicine is rapidly changing in the United States from a cottage industry to one
dominated by large hospital groups and corporations, but the new efficiencies
can be accompanied by a telling loss of intimacy between doctors and patients.
And no specialty has suffered this loss more profoundly than psychiatry.
Trained as a traditional psychiatrist at Michael Reese Hospital, a sprawling
Chicago medical center that has since closed, Dr. Levin, 68, first established a
private practice in 1972, when talk therapy was in its heyday.
Then, like many psychiatrists, he treated 50 to 60 patients in once- or
twice-weekly talk-therapy sessions of 45 minutes each. Now, like many of his
peers, he treats 1,200 people in mostly 15-minute visits for prescription
adjustments that are sometimes months apart. Then, he knew his patients’ inner
lives better than he knew his wife’s; now, he often cannot remember their names.
Then, his goal was to help his patients become happy and fulfilled; now, it is
just to keep them functional.
Dr. Levin has found the transition difficult. He now resists helping patients to
manage their lives better. “I had to train myself not to get too interested in
their problems,” he said, “and not to get sidetracked trying to be a
semi-therapist.”
Brief consultations have become common in psychiatry, said Dr. Steven S.
Sharfstein, a former president of the American Psychiatric Association and the
president and chief executive of Sheppard Pratt Health System, Maryland’s
largest behavioral health system.
“It’s a practice that’s very reminiscent of primary care,” Dr. Sharfstein said.
“They check up on people; they pull out the prescription pad; they order tests.”
With thinning hair, a gray beard and rimless glasses, Dr. Levin looks every bit
the psychiatrist pictured for decades in New Yorker cartoons. His office, just
above Dog Daze Canine Hair Designs in this suburb of Philadelphia, has matching
leather chairs, and African masks and a moose head on the wall. But there is no
couch or daybed; Dr. Levin has neither the time nor the space for patients to
lie down anymore.
On a recent day, a 50-year-old man visited Dr. Levin to get his prescriptions
renewed, an encounter that took about 12 minutes.
Two years ago, the man developed rheumatoid arthritis and became severely
depressed. His family doctor prescribed an antidepressant, to no effect. He went
on medical leave from his job at an insurance company, withdrew to his basement
and rarely ventured out.
“I became like a bear hibernating,” he said.
Missing the Intrigue
He looked for a psychiatrist who would provide talk therapy, write prescriptions
if needed and accept his insurance. He found none. He settled on Dr. Levin, who
persuaded him to get talk therapy from a psychologist and spent months adjusting
a mix of medications that now includes different antidepressants and an
antipsychotic. The man eventually returned to work and now goes out to movies
and friends’ houses.
The man’s recovery has been gratifying for Dr. Levin, but the brevity of his
appointments — like those of all of his patients — leaves him unfulfilled.
“I miss the mystery and intrigue of psychotherapy,” he said. “Now I feel like a
good Volkswagen mechanic.”
“I’m good at it,” Dr. Levin went on, “but there’s not a lot to master in
medications. It’s like ‘2001: A Space Odyssey,’ where you had Hal the
supercomputer juxtaposed with the ape with the bone. I feel like I’m the ape
with the bone now.”
The switch from talk therapy to medications has swept psychiatric practices and
hospitals, leaving many older psychiatrists feeling unhappy and inadequate. A
2005 government survey found that just 11 percent of psychiatrists provided talk
therapy to all patients, a share that had been falling for years and has most
likely fallen more since. Psychiatric hospitals that once offered patients
months of talk therapy now discharge them within days with only pills.
Recent studies suggest that talk therapy may be as good as or better than drugs
in the treatment of depression, but fewer than half of depressed patients now
get such therapy compared with the vast majority 20 years ago. Insurance company
reimbursement rates and policies that discourage talk therapy are part of the
reason. A psychiatrist can earn $150 for three 15-minute medication visits
compared with $90 for a 45-minute talk therapy session.
Competition from psychologists and social workers — who unlike psychiatrists do
not attend medical school, so they can often afford to charge less — is the
reason that talk therapy is priced at a lower rate. There is no evidence that
psychiatrists provide higher quality talk therapy than psychologists or social
workers.
Of course, there are thousands of psychiatrists who still offer talk therapy to
all their patients, but they care mostly for the worried wealthy who pay in
cash. In New York City, for instance, a select group of psychiatrists charge
$600 or more per hour to treat investment bankers, and top child psychiatrists
charge $2,000 and more for initial evaluations.
When he started in psychiatry, Dr. Levin kept his own schedule in a spiral
notebook and paid college students to spend four hours a month sending out
bills. But in 1985, he started a series of jobs in hospitals and did not return
to full-time private practice until 2000, when he and more than a dozen other
psychiatrists with whom he had worked were shocked to learn that insurers would
no longer pay what they had planned to charge for talk therapy.
“At first, all of us held steadfast, saying we spent years learning the craft of
psychotherapy and weren’t relinquishing it because of parsimonious policies by
managed care,” Dr. Levin said. “But one by one, we accepted that that craft was
no longer economically viable. Most of us had kids in college. And to have your
income reduced that dramatically was a shock to all of us. It took me at least
five years to emotionally accept that I was never going back to doing what I did
before and what I loved.”
He could have accepted less money and could have provided time to patients even
when insurers did not pay, but, he said, “I want to retire with the lifestyle
that my wife and I have been living for the last 40 years.”
“Nobody wants to go backwards, moneywise, in their career,” he said. “Would
you?”
Dr. Levin would not reveal his income. In 2009, the median annual compensation
for psychiatrists was about $191,000, according to surveys by a medical trade
group. To maintain their incomes, physicians often respond to fee cuts by
increasing the volume of services they provide, but psychiatrists rarely earn
enough to compensate for their additional training. Most would have been better
off financially choosing other medical specialties.
Dr. Louisa Lance, a former colleague of Dr. Levin’s, practices the old style of
psychiatry from an office next to her house, 14 miles from Dr. Levin’s office.
She sees new patients for 90 minutes and schedules follow-up appointments for 45
minutes. Everyone gets talk therapy. Cutting ties with insurers was frightening
since it meant relying solely on word-of-mouth, rather than referrals within
insurers’ networks, Dr. Lance said, but she cannot imagine seeing patients for
just 15 minutes. She charges $200 for most appointments and treats fewer
patients in a week than Dr. Levin treats in a day.
“Medication is important,” she said, “but it’s the relationship that gets people
better.”
Dr. Levin’s initial efforts to get insurers to reimburse him and persuade his
clients to make their co-payments were less than successful. His office
assistants were so sympathetic to his tearful patients that they often failed to
collect. So in 2004, he begged his wife, Laura Levin — a licensed talk therapist
herself, as a social worker — to take over the business end of the practice.
Ms. Levin created accounting systems, bought two powerful computers, licensed a
computer scheduling program from a nearby hospital and hired independent
contractors to haggle with insurers and call patients to remind them of
appointments. She imposed a variety of fees on patients: $50 for a missed
appointment, $25 for a faxed prescription refill and $10 extra for a missed
co-payment.
As soon as a patient arrives, Ms. Levin asks firmly for a co-payment, which can
be as much as $50. She schedules follow-up appointments without asking for
preferred times or dates because she does not want to spend precious minutes as
patients search their calendars. If patients say they cannot make the
appointments she scheduled, Ms. Levin changes them.
“This is about volume,” she said, “and if we spend two minutes extra or five
minutes extra with every one of 40 patients a day, that means we’re here two
hours longer every day. And we just can’t do it.”
She said that she would like to be more giving of herself, particularly to
patients who are clearly troubled. But she has disciplined herself to confine
her interactions to the business at hand. “The reality is that I’m not the
therapist anymore,” she said, words that echoed her husband’s.
Drawing the Line
Ms. Levin, 63, maintains a lengthy waiting list, and many of the requests are
heartbreaking. On a January day, a pregnant mother of a 3-year-old called to say
that her husband was so depressed he could not rouse himself from bed. Could he
have an immediate appointment? Dr. Levin’s first opening was a month away.
“I get a call like that every day, and I find it really distressing,” Ms. Levin
said. “But do we work 12 hours every day instead of 11? At some point, you have
to make a choice.”
Initial consultations are 45 minutes, while second and later visits are 15. In
those first 45 minutes, Dr. Levin takes extensive medical, psychiatric and
family histories. He was trained to allow patients to tell their stories in
their own unhurried way with few interruptions, but now he asks a rapid-fire
series of questions in something akin to a directed interview. Even so, patients
sometimes fail to tell him their most important symptoms until the end of the
allotted time.
“There was a guy who came in today, a 56-year-old man with a series of business
failures who thinks he has A.D.D.,” or attention deficit disorder, Dr. Levin
said. “So I go through the whole thing and ask a series of questions about
A.D.D., and it’s not until the very end when he says, ‘On Oct. 28, I thought
life was so bad, I was thinking about killing myself.’ ”
With that, Dr. Levin began to consider an entirely different diagnosis from the
man’s pattern of symptoms: excessive worry, irritability, difficulty falling
asleep, muscle tension in his back and shoulders, persistent financial woes, the
early death of his father, the disorganization of his mother.
“The thread that runs throughout this guy’s life is anxiety, not A.D.D. —
although anxiety can impair concentration,” said Dr. Levin, who prescribed an
antidepressant that he hoped would moderate the man’s anxiety. And he pressed
the patient to see a therapist, advice patients frequently ignore. The visit
took 55 minutes, putting Dr. Levin behind schedule.
In 15-minute consultations, Dr. Levin asks for quick updates on sleep, mood,
energy, concentration, appetite, irritability and problems like sexual
dysfunction that can result from psychotropic medications.
“And people want to tell me about what’s going on in their lives as far as
stress,” Dr. Levin said, “and I’m forced to keep saying: ‘I’m not your
therapist. I’m not here to help you figure out how to get along with your boss,
what you do that’s self-defeating, and what alternative choices you have.’ ”
Dr. Levin, wearing no-iron khakis, a button-down blue shirt with no tie, blue
blazer and loafers, had a cheery greeting for his morning patients before
ushering them into his office. Emerging 15 minutes later after each session, he
would walk into Ms. Levin’s adjoining office to pick up the next chart, announce
the name of the patient in the waiting room and usher that person into his
office.
He paused at noon to spend 15 minutes eating an Asian chicken salad with Ramen
noodles. He got halfway through the salad when an urgent call from a patient
made him put down his fork, one of about 20 such calls he gets every day.
By afternoon, he had dispensed with the cheery greetings. At 6 p.m., his waiting
room empty, Dr. Levin heaved a sigh after emerging from his office with his 39th
patient. Then the bell on his entry door tinkled again, and another patient came
up the stairs.
“Oh, I thought I was done,” Dr. Levin said, disappointed. Ms. Levin handed him
the last patient’s chart.
Quick Decisions
The Levins said they did not know how long they could work 11-hour days. “And if
the stock market hadn’t gone down two years ago, we probably wouldn’t be working
this hard now,” Ms. Levin said.
Dr. Levin said that the quality of treatment he offers was poorer than when he
was younger. For instance, he was trained to adopt an unhurried analytic calm
during treatment sessions. “But my office is like a bus station now,” he said.
“How can I have an analytic calm?”
And years ago, he often saw patients 10 or more times before arriving at a
diagnosis. Now, he makes that decision in the first 45-minute visit. “You have
to have a diagnosis to get paid,” he said with a shrug. “I play the game.”
In interviews, six of Dr. Levin’s patients — their identities, like those of the
other patients, are being withheld to protect their privacy — said they liked
him despite the brief visits. “I don’t need a half-hour or an hour to talk,”
said a stone mason who has panic attacks and depression and is prescribed an
antidepressant. “Just give me some medication, and that’s it. I’m O.K.”
Another patient, a licensed therapist who has post-partum depression worsened by
several miscarriages, said she sees Dr. Levin every four weeks, which is as
often as her insurer will pay for the visits. Dr. Levin has prescribed
antidepressants as well as drugs to combat anxiety. She also sees a therapist,
“and it’s really, really been helping me, especially with my anxiety,” she said.
She said she likes Dr. Levin and feels that he listens to her.
Dr. Levin expressed some astonishment that his patients admire him as much as
they do.
“The sad thing is that I’m very important to them, but I barely know them,” he
said. “I feel shame about that, but that’s probably because I was trained in a
different era.”
The Levins’s youngest son, Matthew, is now training to be a psychiatrist, and
Dr. Donald Levin said he hoped that his son would not feel his ambivalence about
their profession since he will not have experienced an era when psychiatrists
lavished time on every patient. Before the 1920s, many psychiatrists were stuck
in asylums treating confined patients covered in filth, so most of the 20th
century was unusually good for the profession.
In a telephone interview from the University of California, Irvine, where he is
completing the last of his training to become a child and adolescent
psychiatrist, Dr. Matthew Levin said, “I’m concerned that I may be put in a
position where I’d be forced to sacrifice patient care to make a living, and I’m
hoping to avoid that.”
Talk Doesn’t Pay, So
Psychiatry Turns to Drug Therapy, NYT, 5.3.2011,
http://www.nytimes.com/2011/03/06/health/policy/06doctors.html
Getting Someone
to Psychiatric Treatment
Can Be Difficult
and
Inconclusive
January 18, 2011
The New York Times
By A. G. SULZBERGER
and BENEDICT CAREY
TUCSON —What are you supposed to do with someone like Jared L. Loughner?
That question is as difficult to answer today as it was in the years and months
and days leading up to the shooting here that left 6 dead and 13 wounded.
Millions of Americans have wondered about a troubled loved one, friend or
co-worker, fearing not so much an act of violence, but — far more likely —
self-inflicted harm, landing in the streets, in jail or on suicide watch. But
those in a position to help often struggle with how to distinguish ominous
behavior from the merely odd, the red flags from the red herrings.
In Mr. Loughner’s case there is no evidence that he ever received a formal
diagnosis of mental illness, let alone treatment. Yet many psychiatrists say
that the warning sings of a descent into psychosis were there for months, and
perhaps far longer.
Moving a person who is resistant into treatment is an emotional, sometimes
exhausting process that in the end may not lead to real changes in behavior.
Mental health resources are scarce in most states, laws make it difficult to
commit an adult involuntarily, and even after receiving treatment, patients
frequently stop taking their medication or seeing a therapist, believing that
they are no longer ill.
The Virginia Tech gunman was committed involuntarily before killing 32 people in
a 2007 rampage.
With Mr. Loughner, dozens of people apparently saw warning signs: the classmates
who listened as his dogmatic language grew more detached from reality. The
police officers who nervously advised that he could not return to college
without a medical note stating that he was not dangerous. His father, who chased
him into the desert hours before the attack as Mr. Loughner carried a black bag
full of ammunition.
“This isn’t an isolated incident,” said Daniel J. Ranieri, president of La
Frontera Center, a nonprofit group that provides mental health services. “There
are lots of people who are operating on the fringes who I would describe as
pretty combustible. And most of them aren’t known to the mental health system.”
Dr. Jack McClellan, an adult and child psychiatrist at the University of
Washington, said he advises people who are worried that someone is struggling
with a mental disorder to watch for three things — a sudden change in
personality, in thought processes, or in daily living. “This is not about
whether someone is acting bizarrely; many people, especially young people,
experiment with all sorts of strange beliefs and counterculture ideas,” Dr.
McLellan said. “We’re talking about a real change. Is this the same person you
knew three months ago?”
Those who have watched the mental unraveling of a loved one say that recognizing
the signs is only the first step in an emotional, often confusing, process.
About half of people with mental illnesses do not receive treatment, experts
estimate, in part because many of them do not recognize that they even have an
illness.
Pushing such a person into treatment is legally difficult in most states,
especially when he or she is an adult — and the attempt itself can shatter the
trust between a troubled soul and the one who is most desperate to help. Others,
though, later express gratitude.
“If the reason is love, don’t worry if they’ll be mad at you,” said Robbie
Alvarez, 28, who received a diagnosis of schizophrenia after being involuntarily
committed when his increasingly erratic behavior led to a suicide attempt. At
the time, he said, he was living in Phoenix with his parents, who he was
convinced were trying to kill him. In Arizona it is easier to obtain an
involuntary commitment than in many states because anyone can request an
evaluation if they observe behavior that suggests a person may present a danger
or is severely disabled (often state laws require some evidence of imminent
danger to self or others).
But there are also questions about whether the system can accommodate an influx
of new patients. Arizona’s mental health system has been badly strained by
recent budget cuts that left those without Medicaid stripped of most of their
services, including counseling and residential treatment, though eligibility
remains for emergency services like involuntary commitment. And the state is
trying to change eligibility requirements for Medicaid, which would potentially
reduce financing further and leave more with limited services.
Still, people who have been through the experience argue that it is better to
act sooner rather than later. “It’s not easy to know when we could or should
intervene but I would rather err on the side of safety than not,” said H. Clarke
Romans, executive director of the local chapter of the National Alliance on
Mental Illness, an advocacy group, who had a son with schizophrenia.
The collective failure to move Mr. Loughner into treatment, either voluntarily
or not, will never be fully understood, because those who knew the young man
presumably wrestled separately and privately about whether to take action. But
the inaction has certainly provoked second-guessing. Sheriff Clarence Dupnik of
Pima County told CNN last Wednesday that Mr. Loughner’s parents were as shocked
as everyone else. “It’s been very, very devastating for them,” he said. “They
had absolutely no way to predict this kind of behavior.”
Linda Rosenberg, president of the National Council for Community Behavioral
Healthcare, said, “The failure here is that we ignored someone for a long time
who was clearly in tremendous distress.” Ms. Rosenberg, whose group is a
nonprofit agency leading a campaign to teach people how to recognize and respond
to signs of mental illness, added, “He wasn’t someone who could ask for help
because his thinking was affected, and as a community no one said, let’s stop
and make sure he gets help.”
At the University of Arizona, where a nursing student killed three instructors
on campus eight years ago before killing himself, feelings of sadness and anger
initially mixed with some guilt as the university examined the missed warning
signs.
The overhauled process for addressing concerns is now more responsive, even if
there are sometimes false alarms, said Melissa M. Vito, vice president for
student affairs. “I guess I’d rather explain why I called someone’s parents than
why I didn’t do something,” she said.
Many others feel the same way.
Four years ago Susan Junck watched her 18-year-old son return from community
college to their Phoenix home one afternoon and, after preparing a snack,
repeatedly call the police to accuse his mother of poisoning him. She assumed it
was an isolated outburst, maybe connected to his marijuana use. In the coming
months, though, her son’s behavior grew more alarming, culminating in an arrest
for assaulting his girlfriend, who was at the center of a number of his
conspiracy theories.
“I knew something was wrong but I literally just did not understand what,” Ms.
Junck, 49, said in a recent interview. “It probably took a year before I
realized my son has a mental illness. This isn’t drug related, this isn’t bad
behavior, this isn’t teenage stuff. This is a serious mental illness.”
Fearful and desperate, she brought her son to an urgent psychiatric center and —
after a five-hour wait — agreed to sign paperwork to have him involuntarily
committed as a danger to himself or others. Her son screamed for her help as he
was carried off. He was diagnosed with paranoid schizophrenia and remains in a
residential treatment facility.
This week Erin Adams Goldman, a suicide prevention specialist with a mental
health nonprofit organization in Tucson, is teaching the first local installment
of a course that is being promoted around the country called mental health first
aid, which instructs participants how to recognize and respond to the signs of
mental illness.
A central tenet is that if a person has suspicions about mental illness it is
better to open the conversation, either by approaching the individual directly,
someone else who knows the person well or by asking for a professional
evaluation.
“There is so much fear and mystery around mental illness that people are not
even aware of how to recognize it and what to do about it,” Ms. Goldman said.
“But we get a feeling when something is not right. And what we teach is to
follow your gut and take some action.”
A. G. Sulzberger reported from Tucson,
and Benedict Carey from New York.
Getting Someone to
Psychiatric Treatment
Can Be Difficult and Inconclusive,
NYT, 18.1.2011,
http://www.nytimes.com/2011/01/19/us/19mental.html
Revising Book
on Disorders of the Mind
February 10, 2010
The New York Times
By BENEDICT CAREY
Far fewer children would get a diagnosis of bipolar disorder. “Binge eating
disorder” and “hypersexuality” might become part of the everyday language. And
the way many mental disorders are diagnosed and treated would be sharply
revised.
These are a few of the changes proposed on Tuesday by doctors charged with
revising psychiatry’s encyclopedia of mental disorders, the guidebook that
largely determines where society draws the line between normal and not normal,
between eccentricity and illness, between self-indulgence and self-destruction —
and, by extension, when and how patients should be treated.
The eagerly awaited revisions — to be published, if adopted, in the fifth
edition of the Diagnostic and Statistical Manual of Mental Disorders, due in
2013 — would be the first in a decade.
For months they have been the subject of intense speculation and lobbying by
advocacy groups, and some proposed changes have already been widely discussed —
including folding the diagnosis of Asperger’s syndrome into a broader category,
autism spectrum disorder.
But others, including a proposed alternative for bipolar disorder in many
children, were unveiled on Tuesday. Experts said the recommendations, posted
online at DSM5.org for public comment, could bring rapid change in several
areas.
“Anything you put in that book, any little change you make, has huge
implications not only for psychiatry but for pharmaceutical marketing, research,
for the legal system, for who’s considered to be normal or not, for who’s
considered disabled,” said Dr. Michael First, a professor of psychiatry at
Columbia University who edited the fourth edition of the manual but is not
involved in the fifth.
“And it has huge implications for stigma,” Dr. First continued, “because the
more disorders you put in, the more people get labels, and the higher the risk
that some get inappropriate treatment.”
One significant change would be adding a childhood disorder called temper
dysregulation disorder with dysphoria, a recommendation that grew out of recent
findings that many wildly aggressive, irritable children who have been given a
diagnosis of bipolar disorder do not have it.
The misdiagnosis led many children to be given powerful antipsychotic drugs,
which have serious side effects, including metabolic changes.
“The treatment of bipolar disorder is meds first, meds second and meds third,”
said Dr. Jack McClellan, a psychiatrist at the University of Washington who is
not working on the manual. “Whereas if these kids have a behavior disorder, then
behavioral treatment should be considered the primary treatment.”
Some diagnoses of bipolar disorder have been in children as young as 2, and
there have been widespread reports that doctors promoting the diagnosis received
consulting and speaking fees from the makers of the drugs.
In a conference call on Tuesday, Dr. David Shaffer, a child psychiatrist at
Columbia, said he and his colleagues on the panel working on the manual “wanted
to come up with a diagnosis that captures the behavioral disturbance and mood
upset, and hope the people contemplating a diagnosis of bipolar for these
patients would think again.”
Experts gave the American Psychiatric Association, which publishes the manual,
predictably mixed reviews. Some were relieved that the task force working on the
manual — which includes neurologists and psychologists as well as psychiatrists
— had revised the previous version rather than trying to rewrite it.
Others criticized the authors, saying many diagnoses in the manual would still
lack a rigorous scientific basis.
The good news, said Edward Shorter, a historian of psychiatry who has been
critical of the manual, is that most patients will be spared the confusion of a
changed diagnosis. But “the bad news,” he added, “is that the scientific status
of the main diseases in previous editions of the D.S.M. — the keystones of the
vault of psychiatry — is fragile.”
To more completely characterize all patients, the authors propose using measures
of severity, from mild to severe, and ratings of symptoms, like anxiety, that
are found as often with personality disorders as with depression.
“In the current version of the manual, people either meet the threshold by
having a certain number of symptoms, or they don’t,” said Dr. Darrel A. Regier,
the psychiatric association’s research director and, with Dr. David J. Kupfer of
the University of Pittsburgh, the co-chairman of the task force. “But often that
doesn’t fit reality. Someone with schizophrenia might have symptoms of insomnia,
of anxiety; these aren’t the diagnostic criteria for schizophrenia, but they
affect the patient’s life, and we’d like to have a standard way of measuring
them.”
In a conference call on Tuesday, Dr. Regier, Dr. Kupfer and several other
members of the task force outlined their favored revisions. The task force
favored making semantic changes that some psychiatrists have long argued for,
trading the term “mental retardation” for “intellectual disability,” for
instance, and “substance abuse” for “addiction.”
One of the most controversial proposals was to identify “risk syndromes,” that
is, a risk of developing a disorder like schizophrenia or dementia. Studies of
teenagers identified as at high risk of developing psychosis, for instance, find
that 70 percent or more in fact do not come down with the disorder.
“I completely understand the idea of trying to catch something early,” Dr. First
said, “but there’s a huge potential that many unusual, semi-deviant, creative
kids could fall under this umbrella and carry this label for the rest of their
lives.”
Dr. William T. Carpenter, a psychiatrist at the University of Maryland and part
of the group proposing the idea, said it needed more testing. “Concerns about
stigma and excessive treatment must be there,” he said. “But keep in mind that
these are individuals seeking help, who have distress, and the question is,
What’s wrong with them?”
The panel proposed adding several disorders with a high likelihood of entering
the pop vernacular. One, a new description of sex addiction, is
“hypersexuality,” which, in part, is when “a great deal of time is consumed by
sexual fantasies and urges; and in planning for and engaging in sexual
behavior.”
Another is “binge eating disorder,” defined as at least one binge a week for
three months — eating platefuls of food, fast, and to the point of discomfort —
accompanied by severe guilt and plunges in mood.
“This is not the normative overeating that we all do, by any means,” said Dr. B.
Timothy Walsh, a psychiatrist at Columbia and the New York State Psychiatric
Institute who is working on the manual. “It involves much more loss of control,
more distress, deeper feelings of guilt and unhappiness.”
Revising Book on
Disorders of the Mind, NYT, 11.2.2010
http://www.nytimes.com/2010/02/10/health/10psych.html
Brain Power
Surgery for Mental Ills
Offers Hope and Risk
November 27, 2009
The New York Times
By BENEDICT CAREY
One was a middle-aged man who refused to get into the shower. The other was a
teenager who was afraid to get out.
The man, Leonard, a writer living outside Chicago, found himself completely
unable to wash himself or brush his teeth. The teenager, Ross, growing up in a
suburb of New York, had become so terrified of germs that he would regularly
shower for seven hours. Each received a diagnosis of severe obsessive-compulsive
disorder, or O.C.D., and for years neither felt comfortable enough to leave the
house.
But leave they eventually did, traveling in desperation to a hospital in Rhode
Island for an experimental brain operation in which four raisin-sized holes were
burned deep in their brains.
Today, two years after surgery, Ross is 21 and in college. “It saved my life,”
he said. “I really believe that.”
The same cannot be said for Leonard, 67, who had surgery in 1995. “There was no
change at all,” he said. “I still don’t leave the house.”
Both men asked that their last names not be used to protect their privacy.
The great promise of neuroscience at the end of the last century was that it
would revolutionize the treatment of psychiatric problems. But the first real
application of advanced brain science is not novel at all. It is a precise,
sophisticated version of an old and controversial approach: psychosurgery, in
which doctors operate directly on the brain.
In the last decade or so, more than 500 people have undergone brain surgery for
problems like depression, anxiety, Tourette’s syndrome, even obesity, most as a
part of medical studies. The results have been encouraging, and this year, for
the first time since frontal lobotomy fell into disrepute in the 1950s, the Food
and Drug Administration approved one of the surgical techniques for some cases
of O.C.D.
While no more than a few thousand people are impaired enough to meet the strict
criteria for the surgery right now, millions more suffering from an array of
severe conditions, from depression to obesity, could seek such operations as the
techniques become less experimental.
But with that hope comes risk. For all the progress that has been made, some
psychiatrists and medical ethicists say, doctors still do not know much about
the circuits they are tampering with, and the results are unpredictable: some
people improve, others feel little or nothing, and an unlucky few actually get
worse. In this country, at least one patient was left unable to feed or care for
herself after botched surgery.
Moreover, demand for the operations is so high that it could tempt less
experienced surgeons to offer them, without the oversight or support of research
institutions.
And if the operations are oversold as a kind of all-purpose cure for emotional
problems — which they are not, doctors say — then the great promise could
quickly feel like a betrayal.
“We have this idea — it’s almost a fetish — that progress is its own
justification, that if something is promising, then how can we not rush to
relieve suffering?” said Paul Root Wolpe, a medical ethicist at Emory
University.
It was not so long ago, he noted, that doctors considered the frontal lobotomy a
major advance — only to learn that the operation left thousands of patients with
irreversible brain damage. Many promising medical ideas have run aground, Dr.
Wolpe added, “and that’s why we have to move very cautiously.”
Dr. Darin D. Dougherty, director of the division of neurotherapeutics at
Massachusetts General Hospital and an associate professor of psychiatry at
Harvard, put it more bluntly. Given the history of failed techniques, like
frontal lobotomy, he said, “If this effort somehow goes wrong, it’ll shut down
this approach for another hundred years.”
A Last Resort
Five percent to 15 percent of people given diagnoses of obsessive-compulsive
disorder are beyond the reach of any standard treatment. Ross said he was 12
when he noticed that he took longer to wash his hands than most people. Soon he
was changing into clean clothes several times a day. Eventually he would barely
come out of his room, and when he did, he was careful about what he touched.
“It got so bad, I didn’t want any contact with people,” he said. “I couldn’t hug
my own parents.”
Before turning to writing, Leonard was a healthy, successful businessman. Then
he was struck, out of nowhere, with a fear of insects and spiders. He overcame
the phobias, only to find himself with a strong aversion to bathing. He stopped
washing and could not brush his teeth or shave.
“I just looked horrible,” he said. “I had a big, ugly beard. My skin turned
black. I was afraid to be seen out in public. I looked like a street person. If
you were a policeman, you would have arrested me.”
Both tried antidepressants like Prozac, as well as a variety of other
medications. They spent many hours in standard psychotherapy for
obsessive-compulsive disorder, gradually becoming exposed to dreaded situations
— a moldy shower stall, for instance — and practicing cognitive and relaxation
techniques to defuse their anxiety.
To no avail.
“It worked for a while for me, but never lasted,” Ross said. “I mean, I just
thought my life was over.”
But there was one more option, their doctors told them, a last resort. At a
handful of medical centers here and abroad, including Harvard, the University of
Toronto and the Cleveland Clinic, doctors for years have performed a variety of
experimental procedures, most for O.C.D. or depression, each guided by
high-resolution imaging technology. The companies that make some of the devices
have supported the research, and paid some of the doctors to consult on
operations.
In one procedure, called a cingulotomy, doctors drill into the skull and thread
wires into an area called the anterior cingulate. There they pinpoint and
destroy pinches of tissue that lie along a circuit in each hemisphere that
connects deeper, emotional centers of the brain to areas of the frontal cortex,
where conscious planning is centered.
This circuit appears to be hyperactive in people with severe O.C.D., and imaging
studies suggest that the surgery quiets that activity. In another operation,
called a capsulotomy, surgeons go deeper, into an area called the internal
capsule, and burn out spots in a circuit also thought to be overactive.
An altogether different approach is called deep brain stimulation, or D.B.S., in
which surgeons sink wires into the brain but leave them in place. A
pacemaker-like device sends a current to the electrodes, apparently interfering
with circuits thought to be hyperactive in people with obsessive-compulsive
disorder (and also those with severe depression). The current can be turned up,
down or off, so deep brain stimulation is adjustable and, to some extent,
reversible.
In yet another technique, doctors place the patient in an M.R.I.-like machine
that sends beams of radiation into the skull. The beams pass through the brain
without causing damage, except at the point where they converge. There they burn
out spots of tissue from O.C.D.-related circuits, with similar effects as the
other operations. This option, called gamma knife surgery, was the one Leonard
and Ross settled on.
The institutions all have strict ethical screening to select candidates. The
disorder must be severe and disabling, and all standard treatments exhausted.
The informed-consent documents make clear that the operation is experimental and
not guaranteed to succeed.
Nor is desperation by itself sufficient to qualify, said Richard Marsland, who
oversees the screening process at Butler Hospital in Providence, R.I., which
works with surgeons at Rhode Island Hospital, where Leonard and Ross had the
operation.
“We get hundreds of requests a year and do only one or two,” Mr. Marsland said.
“And some of the people we turn down are in bad shape. Still, we stick to the
criteria.”
For those who have successfully recovered from surgery, this intensive screening
seems excessive. “I know why it’s done, but this is an operation that could make
the difference between life and death for so many people,” said Gerry Radano,
whose book “Contaminated: My Journey Out of Obsessive-Compulsive Disorder”
(Bar-le-Duc Books, 2007), recounts her own suffering and long recovery from
surgery. She also has a Web site, freeofocd.com, where people from around the
world consult with her.
But for the doctors running the programs, this screening is crucial. “If
patients are poorly selected or not followed well, there’ll be an increasing
number of bad outcomes, and the promise of this field will wither away,” said
Dr. Ben Greenberg, the psychiatrist in charge of the program at Butler.
Dr. Greenberg said about 60 percent of patients who underwent either gamma knife
surgery or deep brain stimulation showed significant improvement, and the rest
showed little or no improvement. For this article, he agreed to put a reporter
in touch with one — Leonard — who did not have a good experience.
The Danger of Optimism
The true measure of an operation, medical ethicists say, is its overall effect
on a person’s life, not only on specific symptoms.
In the early days of psychosurgery, after World War II, doctors published scores
of papers detailing how lobotomy relieved symptoms of mental distress. In 1949,
the Portuguese neurologist Egas Moniz won the Nobel Prize in medicine for
inventing the procedure.
But careful follow-up painted a darker picture: of people who lost motivation,
who developed the helpless indifference dramatized by the post-op rebel McMurphy
in Ken Kesey’s novel “One Flew Over the Cuckoo’s Nest,” played by Jack Nicholson
in the 1975 movie.
The newer operations pinpoint targets on specific, precisely mapped circuits,
whereas the frontal lobotomy amounted to a crude slash into the brain behind the
eyes, blindly mangling whatever connections and circuits were in the way. Still,
there remain large gaps in doctors’ understanding of the circuits they are
operating on.
In a paper published last year, researchers at the Karolinska Institute in
Sweden reported that half the people who had the most commonly offered
operations for obsessive-compulsive disorder showed symptoms of apathy and poor
self-control for years afterward, despite scoring lower on a measure of O.C.D.
severity.
“An inherent problem in most research is that innovation is driven by groups
that believe in their method, thus introducing bias that is almost impossible to
avoid,” Dr. Christian Ruck, the lead author of the paper, wrote in an e-mail
message. The institute’s doctors, who burned out significantly more tissue than
other centers did, no longer perform the operations, partly, Dr. Ruck said, as a
result of his findings.
In the United States, at least one patient has suffered disabling brain damage
from an operation for O.C.D. The case led to a $7.5 million judgment in 2002
against the Ohio hospital that performed the procedure. (It is no longer offered
there.)
Most outcomes, whether favorable or not, have had less remarkable immediate
results. The brain can take months or even years to fully adjust after the
operations. The revelations about the people treated at Karolinska “underscore
the importance of face-to-face assessments of adverse symptoms,” Dr. Ruck and
his co-authors concluded.
The Long Way Back
Ross said he felt no difference for months after surgery, until the day his
brother asked him to play a video game in the basement, and down the stairs he
went.
“I just felt like doing it,” he said. “I would never have gone down there
before.”
He said the procedure seemed to give the psychotherapy sessions a chance to
work, and last summer he felt comfortable enough to stop them. He now spends his
days studying, going to class, playing the odd video game to relax. He has told
friends about the operation, he said, “and they’re O.K. with it — they know the
story.”
Leonard is still struggling, for reasons no one understands. He keeps odd hours,
working through most nights and sleeping much of the day. He is not unhappy, he
said, but he has the same aversion to washing and still lives like a hermit.
“I still don’t know why I’m like this, and I would still try anything that could
help,” he said. “But at this point, obviously, I’m skeptical of the efficacy of
surgery, at least for me.”
Ms. Radano, who wrote the book about her recovery, said the most important thing
about the surgery was that it gave people a chance. “That’s all people in this
situation want, and I know because I was there,” she said while getting into her
car on a recent afternoon.
On the passenger seat was a container of decontaminating hand wipes. She pointed
and laughed. “See? You’re never completely out.”
Surgery for Mental Ills
Offers Hope and Risk, NYT, 27.11.2009,
http://www.nytimes.com/2009/11/27/health/research/27brain.html

Brendan Smialowski for The New York Times
Dr. Darrel A. Regier
is co-chairman of a panel compiling the latest
Diagnostic and Statistical Manual of Mental Disorders
Psychiatrists Revising the Book
of Human Troubles
NYT
18 December 2008
https://www.nytimes.com/2008/12/18/
health/18psych.html
Psychiatrists
Revising the Book of Human Troubles
December 18, 2008
The New York Times
By BENEDICT CAREY
The book is at least three
years away from publication, but it is already stirring bitter debates over a
new set of possible psychiatric disorders.
Is compulsive shopping a mental problem? Do children who continually recoil from
sights and sounds suffer from sensory problems — or just need extra attention?
Should a fetish be considered a mental disorder, as many now are?
Panels of psychiatrists are hashing out just such questions, and their answers —
to be published in the fifth edition of the Diagnostic and Statistical Manual of
Mental Disorders — will have consequences for insurance reimbursement, research
and individuals’ psychological identity for years to come.
The process has become such a contentious social and scientific exercise that
for the first time the book’s publisher, the American Psychiatric Association,
has required its contributors to sign a nondisclosure agreement.
The debate is particularly intense because the manual is both a medical
guidebook and a cultural institution. It helps doctors make a diagnosis and
provides insurance companies with diagnostic codes without which the insurers
will not reimburse patients’ claims for treatment.
The manual — known by its initials and edition number, DSM-V — often organizes
symptoms under an evocative name. Labels like obsessive-compulsive disorder have
connotations in the wider culture and for an individual’s self-perception.
“This is not cardiology or nephrology, where the basic diseases are well known,”
said Edward Shorter, a leading historian of psychiatry whose latest book,
“Before Prozac,” is critical of the manual. “In psychiatry no one knows the
causes of anything, so classification can be driven by all sorts of factors” —
political, social and financial.
“What you have in the end,” Mr. Shorter said, “is this process of sorting the
deck of symptoms into syndromes, and the outcome all depends on how the cards
fall.”
Psychiatrists involved in preparing the new manual contend that it is too early
to say for sure which cards will be added and which dropped.
The current edition of the manual, which was published in 2000, describes 283
disorders — about triple the number in the first edition, published in 1952.
The scientists updating the manual have been meeting in small groups focusing on
categories like mood disorders and substance abuse — poring over the latest
scientific studies to clarify what qualifies as a disorder and what might
distinguish one disorder from another. They have much more work to do, members
say, before providing recommendations to a 28-member panel that will gather in
closed meetings to make the final editorial changes.
Experts say that some of the most crucial debates are likely to include gender
identity, diagnoses of illness involving children, and addictions like shopping
and eating.
“Many of these are going to involve huge fights, I expect,” said Dr. Michael
First, a professor of psychiatry at Columbia who edited the fourth edition of
the manual but is not involved in the fifth.
One example, Dr. First said, is binge eating, now in the manual’s appendix as a
tentative category.
“A lot of people want that included in the manual,” Dr. First said, “and there’s
some research out there, some evidence that drugs are helpful. But binge eating
is also a normal behavior, and you run the risk of labeling up to 30 percent of
people with a disorder they don’t really have.”
The debate over gender identity, characterized in the manual as “strong and
persistent cross-gender identification,” is already burning hot among
transgender people. Soon after the psychiatric association named the group of
researchers working on sexual and gender identity, advocates circulated online
petitions objecting to two members whose work they considered demeaning.
Transgender people are themselves divided about their place in the manual. Some
transgender men and women want nothing to do with psychiatry and demand that the
diagnosis be dropped. Others prefer that it remain, in some form, because a
doctor’s written diagnosis is needed to obtain insurance coverage for treatment
or surgery.
“The language needs to be reformed, at a minimum,” said Mara Keisling, executive
director of the National Center for Transgender Equity. “Right now, the manual
implies that you cannot be a happy transgender person, that you have to be a
social wreck.”
Dr. Jack Drescher, a New York psychoanalyst and member of the sexual disorders
work group, said that, in some ways, the gender identity debate echoed efforts
to remove homosexuality from the manual in the 1970s.
After protests by gay activists provoked a scientific review, the
“homosexuality” diagnosis was dropped in 1973. It was replaced by “sexual
orientation disturbance” and then “ego-dystonic homosexuality” before being
dropped in 1987.
“You had, in my opinion, what was a social issue, not a medical one; and, in
some sense, psychiatry evolved through interaction with the wider culture,” Dr.
Drescher said.
The American Psychiatric Association says the contributors’ nondisclosure
agreement is meant to allow the revisions to begin without distraction and to
prevent authors from making deals to write casebooks or engage in other projects
based on the deliberations without working through the association.
In a phone interview, Dr. Darrel A. Regier, the psychiatric association’s
research director, who with Dr. David Kupfer of the University of Pittsburgh is
co-chairman of the task force, said that experts working on the manual had
presented much of their work in scientific conferences.
“But you need to synthesize what you’re doing and make it coherent before having
that discussion,” Dr. Regier said. “Nobody wants to put a rough draft or raw
data up on the Web.”
Some critics, however, say the secrecy is inappropriate.
“When I first heard about this agreement, I just went bonkers,” said Dr. Robert
Spitzer, a psychiatry professor at Columbia and the architect of the third
edition of the manual. “Transparency is necessary if the document is to have
credibility, and, in time, you’re going to have people complaining all over the
place that they didn’t have the opportunity to challenge anything.”
Scientists who accepted the invitation to work on the new manual — a prestigious
assignment — agreed to limit their income from drug makers and other sources to
$10,000 a year for the duration of the job. “That’s more conservative” than the
rules at many agencies and universities, Dr. Regier said.
This being the diagnostic manual, where virtually every sentence is likely to be
scrutinized, critics have said that the policy is not strict enough. They have
long suspected that pharmaceutical money subtly influences authors’ decisions.
Industry influence was questioned after a surge in diagnoses of bipolar disorder
in young children. Once thought to affect only adults and adolescents, the
disorder in children was recently promoted by psychiatrists on drug makers’
payrolls.
The team working on childhood disorders is expected to debate the merits of
adding pediatric bipolar as a distinct diagnosis, experts say. It is also
expected to discuss whether Asperger’s syndrome, a developmental disorder,
should be merged with high-functioning autism. The two are virtually identical,
but bear different social connotations.
The same team is likely to make a recommendation on so-called sensory processing
disorder, a vague label for a poorly understood but disabling childhood
behavior. Parent groups and some researchers want recognition in the manual in
order to help raise money for research and obtain insurance coverage of
expensive treatments.
“I know that some are pushing very hard to get that in,” Dr. First said, “and
they believe they have been warmly received. But you just never know for sure,
of course, until the thing is published.”
In all, it is a combination of suspense, mystery and prepublication controversy
that many publishers would die for. The psychiatric association knows it has a
corner on the market and a blockbuster series. The last two editions sold more
than 830,000 copies each.
Psychiatrists Revising the Book of
Human Troubles, NYT, 18.12.2008,
http://www.nytimes.com/2008/12/18/health/18psych.html
Standing
in Someone Else’s Shoes,
Almost for Real
December 2,
2008
The New York Times
By BENEDICT CAREY
From the
outside, psychotherapy can look like an exercise in self-absorption. In fact,
though, therapists often work to pull people out of themselves: to see their
behavior from the perspective of a loved one, for example, or to observe their
own thinking habits from a neutral distance.
Marriage counselors have couples role-play, each one taking the other spouse’s
part. Psychologists have rapists and other criminals describe their crime from
the point of view of the victim. Like novelists or moviemakers, their purpose is
to transport people, mentally, into the mind of another.
Now, neuroscientists have shown that they can make this experience physical,
creating a “body swapping” illusion that could have a profound effect on a range
of therapeutic techniques. At the annual meeting of the Society for Neuroscience
last month, Swedish researchers presented evidence that the brain, when tricked
by optical and sensory illusions, can quickly adopt any other human form, no
matter how different, as its own.
“You can see the possibilities, putting a male in a female body, young in old,
white in black and vice versa,” said Dr. Henrik Ehrsson of the Karolinska
Institute in Stockholm, who with his colleague Valeria Petkova described the
work to other scientists at the meeting. Their full study is to appear online
this week in the journal PLoS One. .
The technique is simple. A subject stands or sits opposite the scientist, as if
engaged in an interview.. Both are wearing headsets, with special goggles, the
scientist’s containing small film cameras. The goggles are rigged so the subject
sees what the scientist sees: to the right and left are the scientist’s arms,
and below is the scientist’s body.
To add a physical element, the researchers have each person squeeze the other’s
hand, as if in a handshake. Now the subject can see and “feel” the new body. In
a matter of seconds, the illusion is complete. In a series of studies, using
mannequins and stroking both bodies’ bellies simultaneously, the Karolinska
researchers have found that men and women say they not only feel they have taken
on the new body, but also unconsciously cringe when it is poked or threatened.
In previous work, neuroscientists have induced various kinds of out-of-body
experiences using similar techniques. The brain is so easily tricked, they say,
precisely because it has spent a lifetime in its own body. It builds models of
the world instantaneously, based on lived experience and using split-second
assumptions — namely, that the eyes are attached to the skull.
Therapists say the body-swapping effect is so odd that it could be risky for
anyone in real mental distress. People suffering from the delusions of
schizophrenia or the grandiose mania of bipolar disorder are not likely to
benefit from more disorientation, no matter the intent.
But those who seek help for relationship problems, in particular, often begin to
moderate their behavior only after they have worked to see the encounters in
their daily life from others’ point of view.
“This is especially true for adolescents, who are so self-involved, and also for
people who come in with anger problems and are more interested in changing
everyone else in their life than themselves,” said Kristene Doyle, director of
clinical services at the Albert Ellis Institute in New York.
One important goal of therapy in such cases, Dr. Doyle said, is to get people to
generate alternative explanations for others’ behavior — before they themselves
react.
The evidence that inhabiting another’s perspective can change behavior comes in
part from virtual-reality experiments. In these studies, researchers create
avatars that mimic a person’s every movement. After watching their “reflection”
in a virtual mirror, people mentally inhabit this avatar at some level,
regardless of its sex, race or appearance. In several studies, for instance,
researchers have shown that white people who spend time interacting virtually as
black avatars become less anxious about racial differences.
Jeremy Bailenson, director of the Virtual Human Interaction Lab at Stanford
University, and his colleague Nick Yee call this the Proteus effect, after the
Greek god who can embody many different self-representations.
In one experiment, the Stanford team found that people inhabiting physically
attractive avatars were far more socially intimate in virtual interactions than
those who had less appealing ones. The effect was subconscious: the study
participants were not aware that they were especially good-looking, or that in
virtual conversations they moved three feet closer to virtual conversation
partners and revealed more about themselves than others did. This confidence
lingered even after the experiment was over, when the virtual lookers picked
more attractive partners as matches for a date.
Similar studies have found that people agree to contribute more to retirement
accounts when they are virtually “age-morphed” to look older; and that they will
exercise more after inhabiting an avatar that works out and loses weight.
Adding a physical body-swapping element, as the Swedish team did, is likely to
amplify such changes. “It has video quality, it looks and feels more realistic
than what we can do in virtual environments, so is likely to be much more
persuasive,” Dr. Bailenson said in a telephone interview.
Perhaps too persuasive for some purposes. “It may be like the difference between
a good book, where you can project yourself into a character by filling in with
your imagination, and a movie, where the specific actor gets in the way of
identifying strongly,” he went on.
And above and beyond any therapeutic purposes, the sensation is downright
strange. In the experiments, said Dr. Ehrsson, the Swedish researcher, “even the
feeling from the squeezing hand is felt in the scientist’s hand and not in your
own; this is perhaps the strangest aspect of the experience.”
Standing in Someone Else’s Shoes, Almost for Real,
NYT,
2.12.2008,
http://www.nytimes.com/2008/12/02/health/02mind.html
Use of Antipsychotics in Children
Is Criticized
November 19, 2008
The New York Times
By GARDINER HARRIS
WASHINGTON — Powerful antipsychotic medicines are being used
far too cavalierly in children, and federal drug regulators must do more to warn
doctors of their substantial risks, a panel of federal drug experts said
Tuesday.
More than 389,000 children and teenagers were treated last year with Risperdal,
one of five popular medicines known as atypical antipsychotics. Of those
patients, 240,000 were 12 or younger, according to data presented to the
committee. In many cases, the drug was prescribed to treat attention deficit
disorders.
But Risperdal is not approved for attention deficit problems, and its risks —
which include substantial weight gain, metabolic disorders and muscular tics
that can be permanent — are too profound to justify its use in treating such
disorders, panel members said.
“This committee is frustrated,” said Dr. Leon Dure, a pediatric neurologist from
the University of Alabama School of Medicine who was on the panel. “And we need
to find a way to accommodate this concern of ours.”
The meeting on Tuesday was scheduled to be a routine review of the pediatric
safety of Risperdal and Zyprexa, popular antipsychotic medicines made,
respectively, by Johnson & Johnson and Eli Lilly & Company. Food and Drug
Administration officials proposed that the committee endorse the agency’s
routine monitoring of the safety of the medicines in children and support its
previous efforts to highlight the drugs’ risks.
But committee members unanimously rejected the agency’s proposals, saying that
far more needed to be done to discourage the medicines’ growing use in children,
particularly to treat conditions for which the medicines have not been approved.
“The data show there is a substantial amount of prescribing for attention
deficit disorder, and I wonder if we have given enough weight to the
adverse-event profile of the drug in light of this,” Dr. Daniel Notterman, a
senior health policy analyst at Princeton University and a panel member, said
when speaking about Risperdal.
Drug agency officials responded that they had already placed strongly worded
warnings on the drugs’ labels.
“I’m a little puzzled about the statement that the label is inadequate,” said
Dr. Thomas Laughren, director of the agency’s division of psychiatry products.
“I’m anxious to hear what more we can do in the labeling.”
Kara Russell, a spokeswoman for Johnson & Johnson, said, “Adverse drug reactions
associated with Risperdal use in approved indications are accurately reflected
in the label.”
But panelists said the current warnings were not enough.
While panel members spoke at length about Risperdal, they said their concerns
applied to the other medicines in its class, including Zyprexa, Seroquel,
Abilify and Geodon.
The committee’s concerns are part of a growing chorus of complaints about the
increasing use of antipsychotic medicines in children and teenagers.
Prescription rates for the drugs have increased more than fivefold for children
in the past decade and a half, and doctors now use the drugs to settle outbursts
and aggression in children with a wide variety of diagnoses, even though
children are especially susceptible to their side effects.
A consortium of state Medicaid directors is evaluating the use of the drugs in
children on state Medicaid rolls to ensure that they are being properly
prescribed.
The growing use of the medicines has been driven partly by the sudden popularity
of the diagnosis of pediatric bipolar disorder.
The leading advocate for the bipolar diagnosis is Dr. Joseph Biederman, a child
psychiatrist at Harvard University whose work is under a cloud after a
Congressional investigation revealed that he had failed to report to his
university at least $1.4 million in outside income from the makers of
antipsychotic medicines.
In the past year, Risperdal prescriptions to patients 17 and younger increased
10 percent, while prescriptions among adults declined 5 percent. Most of the
pediatric prescriptions were written by psychiatrists.
From 1993 through the first three months of 2008, 1,207 children given Risperdal
suffered serious problems, including 31 who died. Among the deaths was a
9-year-old with attention deficit problems who suffered a fatal stroke 12 days
after starting therapy with Risperdal.
At least 11 of the deaths were children whose treatment with Risperdal was
unapproved by the F.D.A. Once the agency approves a medicine for a particular
condition, doctors are free to prescribe it for other problems.
Panel members said they had for years been concerned about the effects of
Risperdal and similar medicines, but F.D.A. officials said no studies had been
done to test the drugs’ long-term safety.
Dr. Dure said he was concerned that doctors often failed to recognize the
movement disorders, including tardive dyskinesia and dystonia, that can result
from using these medicines.
“I have a bias that extra-pyramidal side effects are being under-recognized with
these agents,” Dr. Dure said.
Dr. Laughren of the F.D.A. said the agency could do little to fix the problem.
Instead, he said, medical specialty societies must do a better job educating
doctors about the drugs’ side effects.
Use of Antipsychotics
in Children Is Criticized, NYT, 19.11.2008,
http://www.nytimes.com/2008/11/19/health/policy/19fda.html
Daring
to Think Differently
About Schizophrenia
February
24, 2008
The New York Times
By ALEX BERENSON
NORTH
WALES, Pa. — SCIENTISTS who develop drugs are familiar with disappointment —
brilliant theories that don’t pan out or promising compounds derailed by
unexpected side effects. They are accustomed to small steps and wrong turns, to
failure after failure — until, in a moment, with hard work, brainpower and a lot
of luck, all those little failures turn into one big success.
For Darryle D. Schoepp, that moment came one evening in October 2006, while he
was seated at his desk in Indianapolis.
At the time, he was overseeing early-stage neuroscience research at Eli Lilly &
Company and colleagues had just given him the results from a human trial of a
new schizophrenia drug that worked differently than all other treatments. From
the start, their work had been a long shot. Schizophrenia is notoriously
difficult to treat, and Lilly’s drug — known only as LY2140023 — relied on a
promising but unproved theory about how to combat the disorder.
When Dr. Schoepp saw the results, he leapt up in excitement. The drug had
reduced schizophrenic symptoms, validating the efforts of hundreds of
scientists, inside and outside of Lilly, who had labored together for almost two
decades trying to unravel the disorder’s biological underpinnings.
The trial results were a major breakthrough in neuroscience, says Dr. Thomas R.
Insel, director of the National Institute of Mental Health. For 50 years, all
medicines for the disease had worked the same way — until Dr. Schoepp and other
scientists took a different path.
“This drug really looks like it’s quite a different animal,” Dr. Insel says.
“This is actually pretty innovative.”
Dr. Schoepp and other scientists had focused their attention on the way that
glutamate, a powerful neurotransmitter, tied together the brain’s most complex
circuits. Every other schizophrenia drug now on the market aims at a different
neurotransmitter, dopamine.
The Lilly results have fueled a wave of pharmaceutical industry research into
glutamate. Companies are searching for new treatments, not just for
schizophrenia, but also for depression and Alzheimer’s disease and other unseen
demons of the brain that torment tens of millions of people worldwide.
Driving the industry’s interest is the huge market for drugs for brain and
psychiatric diseases. Worldwide sales total almost $50 billion annually, even
though existing medicines have moderate efficacy and have side effects that
range from reduced libido to diabetes.
The glutamate researchers warn that their quest for new treatments for
schizophrenia is far from complete. The results of the Lilly trial covered only
196 patients and must be validated by much larger trials, the last of which may
not be finished until at least 2011. Other glutamate drugs are even further away
from approval. And even if the drugs win that approval, they may be viewed
skeptically by doctors who have been disappointed by side effects in other drugs
that were once been hailed as breakthroughs.
Still, for Dr. Schoepp, the drug’s progress so far is cause for celebration —
and relief.
“I don’t think people appreciate how much money, time and good technical
research goes into what we do,” he says. “Sometimes, people think the idea is
the thing. I think the idea can be the easy part.”
LILLY continues to develop LY2140023 and has begun a trial of 870 patients that
is scheduled to be completed in January 2009. But Dr. Schoepp is no longer
involved in its development. He left Lilly in April to become senior vice
president and head of neuroscience research at Merck, where he oversees a
division of 300 researchers and support staff members.
Dr. Schoepp’s new base is a modest office on the top floor of a four-story Merck
building here in North Wales, north of Philadelphia. He has a view of the
building’s big front lawn and a busy two-lane road called the Sumneytown Pike.
The huge Merck research complex called West Point, where 4,000 scientists and
support staff members work, is less than a mile to the north.
For Dr. Schoepp, 52, the Merck job is the latest stop in a research career that
began at Osco Drug’s store No. 807 in downtown Bismarck, N.D. He grew up in
Bismarck in a working-class family; at 16, he started working at the Osco, which
has since closed. He quickly decided to become a scientist.
“I just found it fascinating,” he says. “I was hungry for science.” While
reading a magazine for pharmacists, he noticed an ad for a free pamphlet
published by Merck called “Pharmacists in Industry.” He wrote away for the
pamphlet, which convinced him that he could have a career developing medicines.
He applied to North Dakota State University, where he focused on
psychopharmacology, a discipline that studies the way chemicals affect the
brain. “I was really interested in psychiatric disorders,” he says. “I fell in
love with dopamine.”
His love affair was so consuming that his wife joked that “dopamine” would be
his daughter’s first word.
Although scientists sometimes decide to study a disease because of problems it
has caused among family members, Dr. Schoepp says his fascination with mental
illness has been purely academic. “My family has more heart disease than
anything else,” he says.
After graduating from North Dakota State, he received a scholarship to a
doctoral program in pharmacology and toxicology at West Virginia University. He
graduated in 1982. Nearly five years later, he joined Lilly, which was about to
introduce Prozac, the first modern antidepressant — a drug that changed both
psychiatry and the public perception of depression and mental illness.
Prozac became a blockbuster almost instantly after Lilly introduced it in 1987,
making the company one of the most visible players in Big Pharma and giving it
room to invest in long-shot scientific research. Ray Fuller, a Lilly scientist
who was a co-discoverer of Prozac, encouraged Dr. Schoepp to focus his attention
on glutamate.
Glutamate is a pivotal transmitter in the brain, the crucial link in circuits
involved in memory, learning and perception. Too much glutamate leads to
seizures and the death of brain cells. Excessive glutamate release is also one
of the main reasons that people have brain damage after strokes. Too little
glutamate can cause psychosis, coma and death.
“The main thoroughfare of communication in the brain is glutamate,” says Dr.
John Krystal, a psychiatry professor at Yale and a research scientist with the
VA Connecticut Health Care System.
Along with Bita Moghaddam, a neuroscientist who was at Yale and is now at the
University of Pittsburgh, Dr. Krystal has been responsible for some of the
fundamental research into how glutamate works in the brain and how it may be
implicated in schizophrenia.
Schizophrenia affects about 2.5 million Americans, about 1 percent of the adult
population, and it usually develops in the late teens or early to mid-20s. It is
believed to result from a mix of causes, including genetic and environmental
triggers that cause the brain to develop abnormally.
The first schizophrenia medicines were developed accidentally about a
half-century ago, when Henri Laborit, a French military surgeon, noticed that an
antinausea drug called chlorpromazine helped to control hallucinations in
psychotic patients. Chlorpromazine, sold under the brand name Thorazine, blocks
the brain’s dopamine receptors. That led the way in the 1960s for drug companies
to introduce other medicines that worked the same way.
The medicines, called antipsychotics, gave many patients relief from the worst
of their hallucinations and delusions. But they also can cause shaking,
stiffness and facial tics, and did not help the cognitive problems or the
so-called negative symptoms like social withdrawal associated with
schizophrenia.
In the 1980s, drug companies looked for new ways to treat the disease with fewer
side effects. By the mid-1990s, they had introduced several new schizophrenia
medicines, including Zyprexa, from Lilly, and Risperdal, from Johnson & Johnson.
At the time, the new medicines were hailed as a major advance — and the
companies marketed them that way to doctors and patients.
In fact, the new medicines, called second-generation antipsychotics, had much in
common with the older drugs. Both worked mainly by blocking dopamine and had
little effect on negative or cognitive symptoms. The newer medicines caused
fewer movement disorders, but had side effects of their own, including huge
weight gain for many patients. Many doctors now complain that the companies
oversold the second-generation compounds and that new treatments are badly
needed.
“People say that there are drugs to treat schizophrenia,” says Dr. Carol A.
Tamminga, professor of psychiatry at the University of Texas Southwestern, in
Dallas. “In fact, the treatment for schizophrenia is at best partial and
inadequate. You have a cadre of cognitively impaired people who can’t fit in.”
WHILE most of the industry focused on second-generation medicines during the
1980s and 1990s, a handful of academic and industry researchers found intriguing
hints that glutamate might provide an alternative treatment pathway.
Psychiatrists and neuroscientists have wondered about a possible connection
between glutamate and schizophrenia since the early ’80s, when they first
learned that phencyclidine, the street drug commonly called PCP, blocks the
release of glutamate.
People who use PCP often have the hallucinations, delusions, cognitive problems
and emotional flatness that are characteristic of schizophrenia. Psychiatrists
noted PCP’s side effects as early as the late 1950s. But they lacked the tools
to determine how PCP affected the brain until 1979, when they found that it
blocked a glutamate receptor, called the NMDA receptor, that is at the center of
the transmission of nerve impulses in the brain.
The PCP finding led a few scientists to begin researching glutamate’s role in
psychosis and other brain disorders. By the early 1990s, they discovered that
besides triggering the primary glutamate receptors — NMDA and AMPA — glutamate
also triggered several other receptors.
They called these newly found receptors “metabotropic,” because the receptors
modified the amount of glutamate that cells released rather than simply turning
circuits on or off. Because glutamate is so central to the brain’s activity,
directly blocking or triggering the NMDA and AMPA receptors can be very
dangerous. The metabotropic receptors appeared to be better targets for drug
treatment.
“Rather than acting as an all-or-nothing signal, they fine-tune that signal and
modulate that signal,” said P. Jeffrey Conn, director of a Vanderbilt University
drug research program. “It’s really an attempt to be very subtle in the way that
you regulate the system.”
During the 1990s, molecular biologists discovered genes for eight metabotropic
glutamate receptors, which were located at different places inside nerve cells
and had different structures. The finding allowed for the possibility that drug
companies could create chemicals to turn them on and off selectively, rather
than hitting all of them at once.
For Dr. Schoepp and others, finding the receptors was only the first part of the
struggle. They also had to find chemicals that would either block or trigger the
receptors selectively. At the same time, the chemicals had to be relatively easy
to formulate and capable of crossing the blood-brain barrier, which protects the
brain from being easily penetrated by outside agents.
The work was arduous, but the Lilly scientists made slow progress. In 1999, Dr.
Schoepp and two other scientists published a 46-page research paper that
detailed scores of different chemicals that produced reactions at the glutamate
sites.
At about the same time, scientists at Yale, led by Dr. Moghaddam, were
demonstrating that activating metabotropic glutamate receptors in rats could
reverse the effects of PCP — a seminal finding, providing the first proof that
altering the path of glutamate transmission in the brain might help relieve the
symptoms of psychosis.
Although the finding in rats was promising, developing animal models for
schizophrenia and other brain diseases is extremely difficult, said Paul
Greengard, professor of molecular and cellular neuroscience at Rockefeller
University.
Even when compared with diseases like cancer, brain disorders are notoriously
complex. Scientists have only a limited understanding of the chemistry of
consciousness, or of how problems in the brain’s electrical circuitry affect the
ability to form memories, learn or think.
“We do not know with any of these neuropsychiatric disorders what the ultimate
basis is,” Dr. Greengard says. “Let’s say you could find that too much of
protein X was involved in schizophrenia. Would you then know what schizophrenia
is? You would not.”
Nonetheless, the findings in rats were promising. Those studies, as well as Dr.
Krystal’s tests in 2001 of volunteers given ketamine, a drug that has effects
similar to PCP, hinted that the glutamate drugs might help to treat the
cognitive and negative symptoms of schizophrenia. Drugs currently on the market
do little to treat those symptoms.
Even before the findings at Yale, Lilly had put its first metabotropic glutamate
receptor compound into human testing. Researchers initially tested the drug on
patients with panic disorder, and it showed some positive results. But Lilly
stopped human testing of the drug in 2001 when long-term testing in animals
showed that it caused seizures.
Even so, Lilly decided that it had enough evidence to justify tests of another
chemical compound, LY404039, that affected the same receptors.
“They had to take a risk on letting these drugs be tested on models or for
disorders that were justified purely on pretty basic science,” Dr. Krystal says.
“There is nothing with these drugs that is straightforward or makes developing
them a basic path.”
When it tried to test LY404039 in humans, the company ran into yet another
hurdle. The human body didn’t easily absorb it. So Lilly created a drug that the
body could absorb, LY2140023, which is metabolized into LY404039 in the body.
Bingo. LY2140023 was the drug that got Dr. Schoepp jumping out of his office
chair in 2006, nearly three years after the first trials in humans began. In the
Lilly test, the drug was slightly less effective over all than Zyprexa, which is
considered the most effective among the widely used schizophrenia treatments.
But LY2140023 also appeared to have fewer side effects than Zyprexa, which can
cause severe weight gain and diabetes. The new drug also appeared to improve
cognition, something that existing treatments don’t do, said Dr. Insel of the
National Institute of Mental Health.
IF Lilly’s new round of tests confirms the drug’s efficacy by early next year,
the company is likely to move ahead to an even larger clinical trial, involving
thousands of patients, that could lead to federal approval for the compound.
Still, approval is at least three to four years away, and other big drug makers
are already scrambling to compete with Lilly.
In January, Pfizer agreed to pay Taisho Pharmaceutical, a Japanese company, $22
million for the rights to develop Taisho’s glutamate drug for schizophrenia.
Taisho will receive more payments if the drug moves forward in development.
Since it hired Dr. Schoepp, Merck has also been moving aggressively. It has
struck two deals since December to work with Addex Pharmaceuticals, a Swiss
company, to develop glutamate drugs for schizophrenia, Parkinson’s and other
diseases. Merck has paid Addex $25 million so far, with more payments to come if
the drugs move forward.
Another glutamate drug, meanwhile, has been shown in preclinical studies to
reverse mental retardation in adult rats, a finding that previously appeared
impossible, Dr. Insel said.
Dr. Steven M. Paul, the president of Lilly Research Laboratories, says Lilly
expects competition in glutamate research to intensify. “We’d like to believe we
have a head start here, and hopefully a good head start,” he says. “But this
area will heat up here; this will be an area where there will be a lot of
investment.”
For Dr. Schoepp, the sudden interest in glutamate is exciting, and he
acknowledges that he eagerly awaits the results of the large Lilly trial early
next year. And what if the drug fails in that trial, after all the work that he
and scientists around the world have put in?
“I would probably go out and have a beer,” he says. “You have to define failure.
If you collect information and it tells you what you need to know, you’re not a
failure.”
Daring to Think Differently About Schizophrenia, NYT,
24.2.2008,
http://www.nytimes.com/2008/02/24/business/24drug.html
Vicious
Killing
Where Troubled Seek a Listener
February
14, 2008
The New York Times
By AL BAKER
It was just
after 8 p.m. in a suite of mental health offices at East 79th Street and York
Avenue. One doctor was seeing patients; another was working in her study.
It is a common scene in the offices of countless Manhattan therapists after
dark: The lights stay on as paperwork is done and patients are treated into the
evening.
Then a middle-aged man in a black cap and sneakers came in from the freezing
rain, toting two pieces of black luggage. He said he was there to see a
psychiatrist named Kent D. Shinbach. But Dr. Shinbach had another patient, a
woman, waiting for him, so the man sat on a couch and made small talk. Then he
disappeared into the office of the other doctor, Kathryn Faughey, the police
said.
And there — in what investigators described as a furious swirl of violence on
Tuesday night — the man stabbed Dr. Faughey in the head, face and chest. Hearing
her screams, Dr. Shinbach rushed in and saw her lying still and bleeding on the
tan carpet by the foot of her desk.
The attacker turned on him, stabbing him in the face, head and hands, the police
said. Dr. Faughey, 56, was declared dead at the scene; Dr. Shinbach, who is in
his 70s, survived, but was left in critical condition.
A day later, the police said they did not know the motive for the frenzied
attack nor the identity of the killer, though investigators are pursuing the
possibility that he was a patient at the offices, where five health care
professionals work, or that he was a relative of a patient there or was somehow
involved with one.
But even before a motive had been determined, psychiatrists, psychologists and
social workers who work in Manhattan — a place long linked in the public
imagination with the stereotypical image of an urbanite on a couch discussing
his worries — reacted with alarm. Several said the violence in the office at 435
East 79th Street reminded them of the dangers inherent in a career spent helping
people, particularly those in emotional pain.
Dr. Faughey grew up in Sunnyside, Queens, and lived across the street from her
office. Her husband of 25 years, Walter Adam, said he became worried about 8:30
p.m. because his wife was late. He looked out the window of their 17th-floor
apartment and noticed that the light was still on in her office. He called and
got no answer. Then he saw police cars on the block.
“I thought it was an automobile accident,” he said. “Finally I said, ‘I better
go over and see what’s going on.’ ”
He heard the news from a police officer: His wife had been killed.
“She’s taken very good care of me,” Mr. Adam said. “She’s looked after me. She’s
a good and decent woman. Never harmed anyone.”
Police Commissioner Raymond W. Kelly said that after stabbing both doctors, the
attacker pinned Dr. Shinbach against the wall with a spindled chair, took $90
from his wallet and fled to the building’s neatly painted basement and out a
service exit. He left his two suitcases behind in the basement, where the police
found a smear of blood on the door. The woman who had been waiting to see Dr.
Shinbach had gone into his office at one point and was unharmed.
During the attack on Dr. Shinbach, which lasted about 10 minutes, the attacker
told him, “She’s dead,” the police said, adding that other comments he made did
not shed light on his actions.
Mr. Kelly said a key part of the investigation was to determine whether the
killer “was a patient of any of the health care professionals in that suite of
offices.”
Three knives were later found: one at Dr. Faughey’s left foot; another, a 9-inch
blade that was bent in the attack, underneath her desk; and a meat cleaver, also
bent and with a broken handle, lying in front of a wall of books. Blood was
splashed on the walls and floor. “It was obvious a fierce struggle had taken
place,” said Paul J. Browne, the Police Department’s chief spokesman.
Investigators found that the larger suitcase, which had wheels and a handle,
held women’s slippers and a blouse, as well as disposable diapers for adults.
Inside the smaller bag were eight knives — mostly kitchen knives — three lengths
of rope and rolls of duct tape.
Dr. Faughey received a doctorate in clinical psychology from the Ferkauf
Graduate School of Psychology at Yeshiva University in 1981. She had been
practicing cognitive behavior psychotherapy on the Upper East Side for more than
20 years, according to her Web site.
“My approach is focused and solution-oriented,” according to a quotation on the
site. “My sessions move quickly. I am interactive, and I give feedback.”
Mr. Adam said his wife achieved tremendous results for her patients. “The way
she turned around people’s lives, saved people’s lives,” he said.
“She was always a person who was reading and studying,” said Kevin Faughey, Dr.
Faughey’s oldest brother and one of her six siblings. “She always had goals in
her life that she wanted to do something for humanity, in some way, shape or
form to help.”
Dr. Shinbach has admitted patients to Beth Israel Medical Center and Gracie
Square Hospital, said Dr. Michael Serby, an associate chairman of Beth Israel.
“Clearly he’s a brave individual and a hero.”
Dr. Frederick J. Long, a Manhattan psychiatrist who has known Dr. Shinbach for
14 years, described him as dedicated and caring. “He is the best mentor I’ve
ever had,” Dr. Long said, adding that Dr. Shinbach was among the first
psychiatrists to take an interest in elderly patients.
Another colleague said Dr. Shinbach’s relationship with Dr. Faughey was limited
to the shared office space; they did not see each other’s patients.
The attacker’s entrance and departure were captured by security cameras. He
arrived at the first-floor offices just after 8 p.m. He left at 8:59 p.m.
through the basement door, on which investigators found blood. Investigators
said the attacker might have cut his hand. It is common in such furious attacks,
when blood can make the weapons slick. The police said DNA tests would be
conducted to determine whose the blood was, but it was unclear how long the
tests would take.
In the videotape, the man’s arrival is seen as a doorman holds a glass door open
for him; he briskly walks in, stating that he was there to see Dr. Shinbach.
Pulling his bags, he then goes up a short set of steps from the lobby to the
professional offices.
The videotape of the man leaving shows him from behind, as he rounds a corner in
the basement and disappears out the exit, onto 79th Street between First and
York Avenues. The police are checking security videos from businesses in the
area to see if they can pick up images of him.
At a news conference, Mr. Kelly held up a sketch of the suspect that was based
on descriptions provided by witnesses who saw the man before the attack.
Dr. Shinbach, who was interviewed by detectives after undergoing surgery at
NewYork-Presbyterian Hospital/Weill Cornell Medical Center, did not recognize
his attacker.
Mr. Kelly described the killer as a man in his 40s, about 5-foot-9, with
brownish or blond hair. He was wearing a three-quarter-length green coat and
sneakers. A baseball cap believed to be the killer’s was found in Dr. Faughey’s
office, the police said.
After the attack, Dr. Shinbach yelled for help from Dr. Faughey’s office window.
The building’s doorman had left just left on a break and heard his cries.
Later, the doorman, Frank Batista, said he was almost certain he could identify
the attacker — “99.9 percent.”
Reporting was contributed by John Eligon, Dmitry Kiper,
Robin Stein, Stacey
Stowe, Andrew Tangel
and Carolyn Wilder.
Vicious Killing Where Troubled Seek a Listener, NYT,
14.2.2008,
https://www.nytimes.com/2008/02/14/
nyregion/14slay.html
Working
in Mental Health,
the Prospect of Violence
Is a Part of the Job
February
14, 2008
The New York Times
By JAMES BARRON
Therapists
— psychiatrists, psychotherapists, psychiatric social workers and other mental
health professionals — are as much part of the New York landscape as hot dog
vendors. And they have discovered, sometimes the hard way, that delving deeply
into people’s feelings can be dangerous.
As police detectives searched on Wednesday for a man who killed a psychologist
with a meat cleaver and other knives — and seriously injured another therapist,
who heard their struggle from his nearby office and went to help — therapists
said they had learned to develop their own physical and psychological defenses
against violence.
But they conceded that a shrewd and determined attacker who appears normal could
fool them.
“You do this work long enough, and you pretty much see everything, even in
Manhattan,” said Dr. Robert H. Reiner, the executive director of Behavioral
Associates, a private outpatient psychotherapy institute on the Upper East Side.
The identity of the attacker in Tuesday’s killing was not known, and the police
said it was not clear if he was a patient or a patient’s relative, or if he had
some other connection to the victims.
Still, therapists said they recognized the inherent risk in treating some types
of patients. Dr. Reiner said most of the patients he saw, in six to eight
“intake interviews” a day, had anxiety disorders that carried a low risk of
violence. But every so often, he realizes that a patient has a severe psychosis.
“Often as not, it’s someone who’s walking around like you and me, and the
psychosis is well disguised, and I realize they could be dangerous,” Dr. Reiner
said. “And I look at the window and I think, ‘How quick can I get out?’ Every
psychotherapist in an urban area knows this feeling.”
Just how much violence is directed at therapists is an open question. Of a dozen
therapists in private practice in New York City who were interviewed on
Wednesday, only one said he had ever seen violence in his office, and he was not
the target: A father and son came to blows, he said.
But when Christina E. Newhill, an associate professor at the University of
Pittsburgh, surveyed 1,129 therapeutic workers nationwide in 2003, 58 percent
said they had had to deal with violence, though only 24 percent of those said
they had actually been attacked. Twenty-five percent of those who had to deal
with violence said clients had damaged or destroyed property, while half said
the episodes did not go beyond threats.
Gary Arthur, a professor emeritus at Georgia State University, surveyed all
6,400 licensed therapists in Georgia in 2001. Of the 1,132 who responded, 14 had
been shot at, 6 attacked with a knife, 209 pushed or shoved, 112 slapped and 87
hit by objects thrown at them. None of the therapists who said they had been
shot at were struck by the bullets, he said.
“The results were scary,” he said in an interview. “Our profession remains very
high on the list for risk of danger.”
Twice in his years as a psychologist, Dr. Alan Hilfer, now the chief
psychologist at Maimonides Medical Center in Brooklyn, has had to deal with
violent patients: once when a father and son got into a knock-down-drag-out
brawl in his consultation room, and once when a teenager threw a paperweight at
the therapist in the next office.
Dr. Hilfer said therapists were not taught precautions — like where to position
oneself during a consultation — during training.
He recalled being asked, early in his career, to interview a man seeking
treatment. “I allowed him to come between me and the door” in the consultation
room, Dr. Hilfer said. “He became agitated and threatening, and I couldn’t get
out of the room.”
In some group practices or in hospitals, he said, therapists leave the door open
during a first encounter with a patient. They also alert a colleague, who
listens for sounds of a disturbance.
Dr. Newhill teaches a class that tells prospective therapists how to do risk
assessments and handle patients who turn violent. In a telephone interview, she
said she started the class because of a murder in California in 1989. A
therapist at a mental health clinic in Santa Monica was stabbed 31 times in her
office by a patient, a street person who Dr. Newhill said was delusional.
“Violence is an interaction between the person and their environment,” she said,
adding that the best predictor of future violence is a recent history of
violence. She tells her students to work out, in advance, a plan that includes a
way to signal for help. Some therapists install silent alarms. Others work out a
phrase that lets a colleague know help is needed: “Please cancel my appointment
for 3 o’clock” could mean “Call 911,” for example.
Dr. Reiner, of Behavioral Associates, said patients who turn violent had often
“scoped things out in advance.” He said they would figure out whether a
therapist worked alone or in an office with secretaries, other therapists or
even video surveillance cameras.
But therapists who work by themselves, as many do in Manhattan, cannot turn to a
colleague or a subordinate for assistance when a session degenerates.
“There is no warning system” for solo practitioners, Dr. Hilfer said. “We can
try to use our clinical awareness and our knowledge of the patient, and if we
are concerned about a patient, we will send them for a consult with someone. But
in terms of protection, there’s none. It underscores the vulnerability that many
of us understand.”
John Eligon and Anthony Ramirez
contributed reporting.
Working in Mental Health,
the Prospect of Violence Is a
Part of the Job,
NYT, 14.2.2008,
https://www.nytimes.com/2008/02/14/
nyregion/14pysch.html
Explore more on these topics
Anglonautes > Vocapedia
mental health, psychology
war > veterans
negative feelings
feelings > stress, fear, shock
death > suicide >
prevention
death >
suicide
- warning: distressing content
|